The human papillomavirus (HPV) is a highly widespread and intricate group of viruses that can have significant consequences for human health. This article explores the complex world of HPV, including its traits, related health hazards, diagnostic techniques, and the critical role vaccination plays in avoiding diseases linked to HPV.
What is Human Papillomavirus (HPV)?
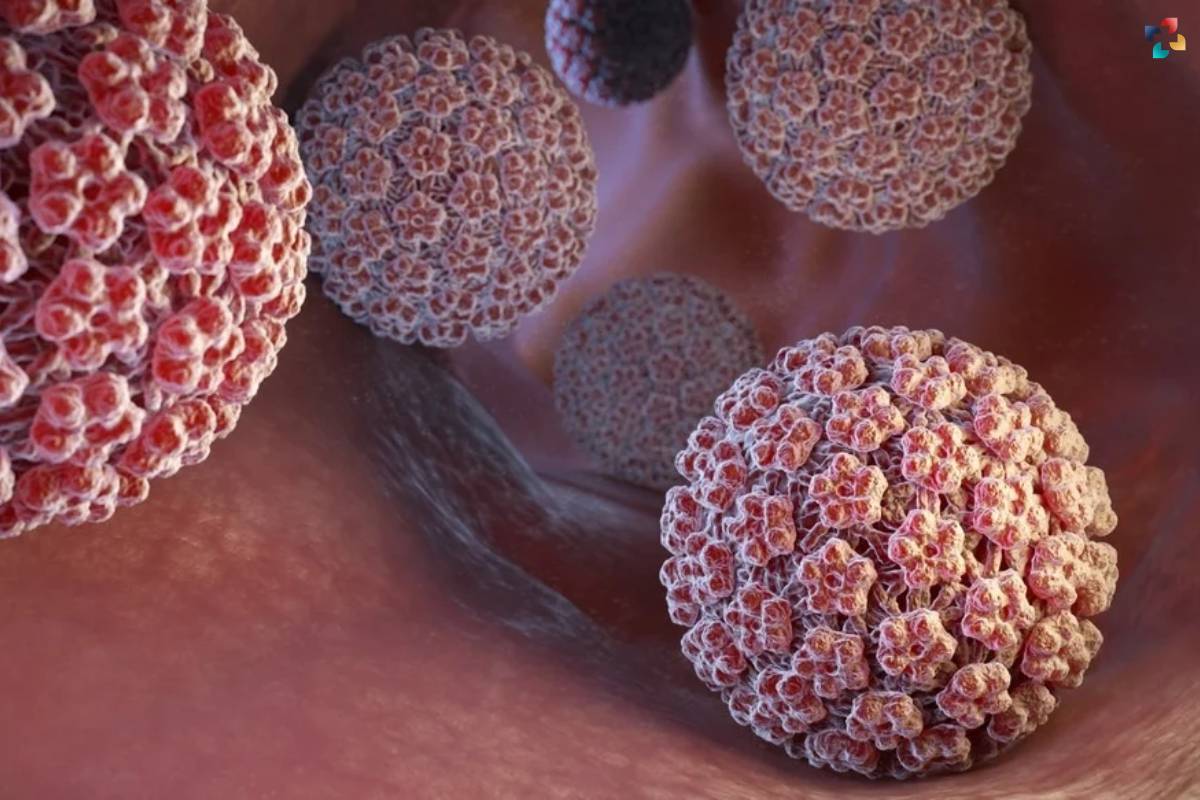
Human Papillomavirus (HPV) stands as a dynamic and diverse family of viruses, offering both benign encounters and the potential for severe health implications. This extensive group comprises over 200 distinct types, each with its unique characteristics, preferences, and consequences upon human infection.
At its core, HPV is a group of DNA viruses that exhibit a predilection for infecting the skin and mucous membranes. These viruses traverse various human tissues, finding residence in areas such as the genital tract, anal canal, mouth, and throat. The modes of transmission are diverse, encompassing intimate skin-to-skin contact, sexual activity, and, in some cases, vertical transmission from an infected mother to her newborn during childbirth.
The classification of HPV into low-risk and high-risk categories serves as a crucial delineation, guiding our understanding of the potential health outcomes associated with different viral strains. Many Human Papillomavirus infections are transient and relatively innocuous, causing no lasting harm to the host. These low-risk types, such as HPV 6 and 11, are often linked to the development of genital warts – non-cancerous growths that, while troublesome, pose minimal long-term health risks.
However, the narrative shifts when high-risk Human Papillomavirus (HPV) types come into play. A subset of these viruses, notably HPV 16 and 18, holds the potential to instigate a cascade of events leading to various cancers. Persistent infection with high-risk HPV strains can result in the development of precancerous lesions, particularly in the cervical epithelium. If left unaddressed, these lesions can progress to invasive cervical cancer, presenting a formidable threat to women’s health globally.
Beyond the cervix, high-risk HPV types contribute to the etiology of other malignancies, including anal and oropharyngeal cancers. The interconnectedness of these viruses with different anatomical sites underscores the need for a comprehensive understanding of HPV’s impact on human health.
It’s essential to acknowledge that the majority of Human Papillomavirus (HPV) infections are transient and resolve spontaneously, thanks to the vigilant immune response of the host. However, the persistence of high-risk types emphasizes the need for proactive measures, including vaccination and regular screenings, to mitigate the potential progression to severe health outcomes.
In unraveling the intricate tapestry of HPV infections, scientists, healthcare professionals, and public health initiatives aim to empower individuals with knowledge and tools for prevention and early intervention. The ongoing exploration of HPV’s nuances not only informs medical practices but also underscores the significance of holistic approaches to public health, where education, vaccination, and timely screenings converge to safeguard individuals from the intricate dance of Human Papillomavirus.
Low-Risk and High-Risk Types of Human Papillomavirus:
Low-Risk HPV Types:
- HPV 6 and 11: These types are most commonly associated with genital warts, which are non-cancerous growths on the genital and anal areas.
- Low-risk mucosal types: Some low-risk types can cause respiratory papillomatosis, leading to the growth of warts in the respiratory tract.
High-Risk HPV Types:
- HPV 16 and 18: These high-risk types are responsible for the majority of HPV-related cancers, including cervical, anal, and oropharyngeal cancers.
- Other high-risk types: HPV 31, 33, 45, 52, and 58 are also associated with an increased risk of cancer development.
Health Risks Associated with Human Papillomavirus (HPV) Infections:
1. Cervical Cancer
HPV and Cervical Cancer: Persistent infection with high-risk HPV types, particularly HPV 16 and 18, is the primary cause of cervical cancer. These viruses can lead to the gradual development of precancerous lesions that may progress to invasive cervical cancer if left untreated.
2. Other HPV-Related Cancers
- Anal Cancer: HPV is a major risk factor for anal cancer, affecting both men and women, particularly those with a history of anal intercourse.
- Oropharyngeal Cancer: Human Papillomavirus, especially type 16, is a significant contributor to oropharyngeal cancers, affecting the base of the tongue and tonsils.
3. Genital Warts:
- Low-Risk Types: HPV 6 and 11 are associated with the development of genital warts, non-cancerous growths that can appear on the genital and anal regions.
Diagnostic Approaches: Unraveling the Presence of HPV
1. Pap Smear and HPV Test:
- Pap Smear: Pap smear, also known as Pap test, is a routine screening method that examines cervical cells for abnormalities. It can detect early signs of cervical cancer or precancerous changes.
- HPV Test: HPV testing involves checking for the presence of high-risk HPV types in cervical cells. This test is often conducted alongside a Pap smear, providing a comprehensive assessment of cervical health.
2. DNA Testing:

- DNA Testing for High-Risk Types: Molecular tests that detect the presence of specific HPV DNA can identify high-risk types associated with cancer development. These tests are often used in conjunction with Pap smears or Human Papillomavirus tests for a more accurate diagnosis.
The Role of HPV Vaccination
1. HPV Vaccine Basics:
- Target Population: HPV vaccines are recommended for both males and females, typically administered during adolescence to provide protection before potential exposure to the virus.
- Vaccine Types: Currently available vaccines target the most common high-risk types (16 and 18) and the most prevalent low-risk types (6 and 11) associated with genital warts.
2. Vaccine Efficacy and Impact:
- Cancer Prevention: Human Papillomavirus vaccination has demonstrated efficacy in preventing HPV-related cancers, including cervical, anal, and oropharyngeal cancers.
- Genital Warts: The vaccine significantly reduces the incidence of genital warts caused by low-risk HPV types.
3. Global Vaccination Initiatives:
- Impact on Cervical Cancer: Countries with high HPV vaccination coverage have observed substantial declines in cervical cancer rates, highlighting the vaccine’s potential to transform public health outcomes globally.

All You Need to Know About HPV and HPV Vaccine
Human Papillomavirus (HPV), is a type of cervical cancer. It is the main cause of the spread of cervical cancer all over the world. It is causing thousands of deaths annually. Regular screening to be sure cervical cancer isn’t affecting us is the best thing to adopt.
Challenges and Future Directions in HPV Control
1. Vaccine Hesitancy:
- Public Perception: Vaccine hesitancy and misinformation pose challenges to achieving high vaccination coverage. Public health campaigns emphasizing the safety and efficacy of HPV vaccines are crucial in addressing these concerns.
2. Global Access:
- Equitable Distribution: Ensuring equitable access to Human Papillomavirus vaccines is essential for global HPV control. Efforts are ongoing to improve access in low-resource settings, where the burden of HPV-related diseases is often higher.
3. Research and Innovation:

- Next-Generation Vaccines: Ongoing research explores the development of next-generation HPV vaccines, addressing a broader range of HPV types and potentially providing broader protection.
Conclusion: A Holistic Approach to HPV Control
With the growing comprehension of the Human Papillomavirus, the significance of a comprehensive strategy for HPV control is becoming more apparent. Our available instruments provide possibilities for early identification and prevention, ranging from effective immunization campaigns to sophisticated diagnostic techniques. Reducing the burden of HPV-related diseases requires worldwide coordination, addressing vaccine reluctance, and placing a strong emphasis on education. A united front among academics, politicians, and healthcare practitioners is essential in navigating the complicated landscape of HPV in order to minimize, if not completely eradicate, HPV-related illnesses and malignancies in the future.