Frontotemporal dementia (FTD) is a progressive neurodegenerative disorder that primarily affects the frontal and temporal lobes of the brain, leading to changes in behavior, personality, and language skills. It is one of the less common types of dementia, but its impact on individuals and their families can be profound. In this comprehensive guide, we’ll delve into the intricacies of Frontotemporal Dementia, exploring its symptoms, causes, diagnosis, and treatment options.
Symptoms of Frontotemporal Dementia:
Frontotemporal Dementia presents with a wide range of symptoms that can vary depending on the subtype of the disease and the areas of the brain affected. Common symptoms include changes in behavior, such as impulsivity, apathy, disinhibition, and loss of empathy. Individuals may also experience language difficulties, including aphasia (difficulty speaking or understanding language) and apraxia (difficulty coordinating movements). As the disease progresses, cognitive decline may occur, leading to memory loss, executive dysfunction, and impaired judgment.
Frontotemporal Dementia (FTD) encompasses a spectrum of symptoms that can manifest differently from person to person. One of the hallmark features of FTD is the early onset of symptoms, typically occurring between the ages of 40 and 65, although cases outside this range are not uncommon.
Behavioral changes are often among the first symptoms noticed by family members and caregivers. Individuals with FTD may exhibit impulsive or socially inappropriate behaviors, such as making tactless comments or acting impulsively in social situations. Apathy, or a lack of interest or motivation, is also common in FTD and can manifest as a loss of interest in previously enjoyed activities or a lack of initiative in completing tasks.
Language difficulties are another prominent feature of FTD, particularly in the primary progressive aphasia (PPA) subtype. Individuals may struggle to find the right words, follow conversations, or comprehend written or spoken language. This can lead to frustration and communication breakdowns in social interactions.
As the disease progresses, cognitive decline becomes more pronounced, affecting memory, executive function, and judgment. Individuals may experience difficulty with tasks that require planning, organization, and decision-making. Memory loss may also become more noticeable, particularly in recalling recent events or learning new information.
Overall, the symptoms of Frontotemporal Dementia can have a significant impact on an individual’s quality of life and ability to function independently. Early recognition and diagnosis are essential for accessing appropriate care and support services to help manage the challenges associated with FTD.
Causes of Frontotemporal Dementia:

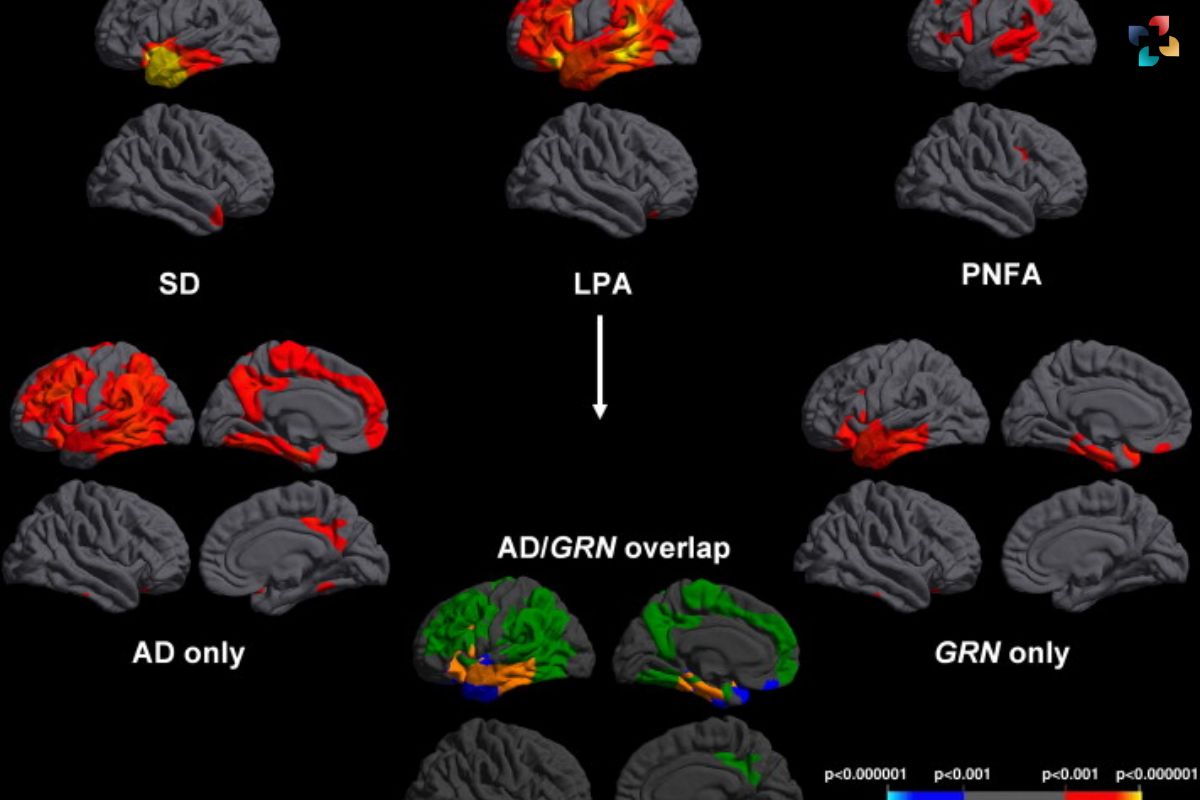
The exact causes of Frontotemporal Dementia are not fully understood, but it is believed to result from a combination of genetic, environmental, and lifestyle factors. Mutations in several genes, including the C9orf72, MAPT, and GRN genes, have been associated with familial forms of FTD. These mutations disrupt normal brain function, leading to the characteristic symptoms of the disease. Environmental factors, such as head trauma and exposure to toxins, may also contribute to the development of FTD.
Diagnosis of Frontotemporal Dementia:
Diagnosing Frontotemporal Dementia can be challenging due to its overlap with other neurodegenerative disorders, such as Alzheimer’s disease and Parkinson’s disease. A comprehensive evaluation, including a thorough medical history, physical examination, neuropsychological testing, and brain imaging studies, is essential for an accurate diagnosis. Genetic testing may also be recommended, especially for individuals with a family history of FTD.
Frontotemporal Dementia (FTD) is often diagnosed through a multi-step process that involves careful evaluation by healthcare professionals with expertise in neurodegenerative disorders. The initial assessment typically begins with a comprehensive medical history to gather information about the individual’s symptoms, family history, and any relevant medical conditions or medications. A thorough physical examination may also be conducted to assess neurological function and rule out other potential causes of symptoms.
Neuropsychological testing is a crucial component of the diagnostic process for FTD. These assessments evaluate various cognitive functions, such as memory, language, executive function, and visuospatial skills, to identify patterns of impairment consistent with FTD. Tests may include tasks to assess verbal fluency, problem-solving abilities, and memory recall, among others.
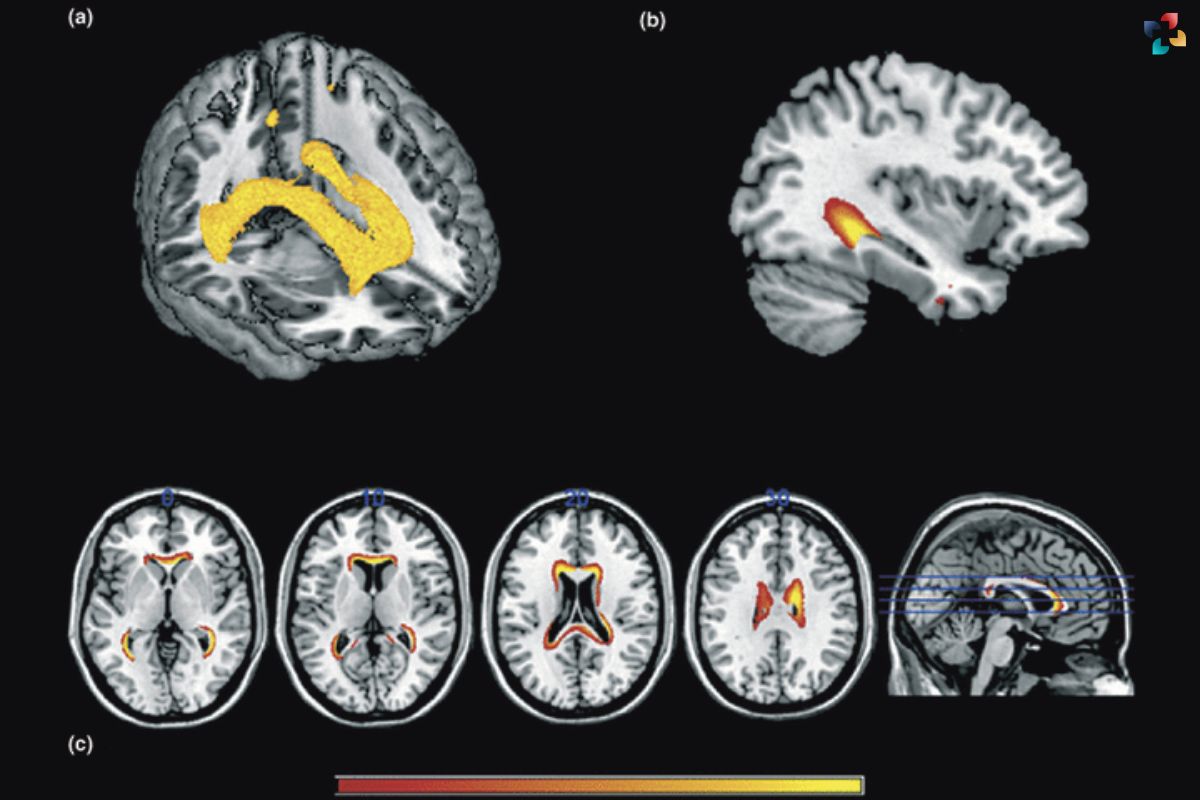
Brain imaging studies, such as magnetic resonance imaging (MRI) or positron emission tomography (PET), may be performed to detect structural changes in the brain associated with FTD. MRI scans can reveal patterns of atrophy (shrinkage) in the frontal and temporal lobes of the brain, which are characteristic of FTD. PET scans may be used to assess metabolic activity or the accumulation of abnormal proteins in the brain, providing additional diagnostic information.
In some cases, genetic testing may be recommended, particularly for individuals with a family history of FTD or known genetic mutations associated with the condition. Identifying specific genetic factors can help confirm a diagnosis of FTD and provide important information about disease prognosis and inheritance patterns for affected individuals and their families.
Overall, the diagnosis of Frontotemporal Dementia requires a comprehensive and multidisciplinary approach to accurately assess symptoms, identify potential underlying causes, and develop an appropriate management plan tailored to the individual’s needs. Early recognition and intervention are critical for optimizing outcomes and providing supportive care to individuals affected by FTD and their families.
Treatment Options for Frontotemporal Dementia:
Currently, there is no cure for Frontotemporal Dementia, and treatment focuses on managing symptoms and improving quality of life. Medications may be prescribed to alleviate behavioral symptoms, such as antidepressants, antipsychotics, and mood stabilizers. Speech and language therapy can help individuals with language difficulties communicate more effectively. Occupational therapy and physical therapy may also be beneficial in maintaining independence and mobility. Additionally, supportive services, such as caregiver support groups and respite care, can provide much-needed assistance for both patients and their families.

In conclusion, Frontotemporal Dementia is a complex and challenging condition that requires comprehensive evaluation and management. By understanding its symptoms, causes, diagnosis, and treatment options, individuals and their families can better cope with the challenges of living with FTD. Ongoing research into the underlying mechanisms of the disease offers hope for future advancements in treatment and ultimately, a cure for Frontotemporal Dementia.
FAQs
What is Frontotemporal Dementia (FTD)?
Frontotemporal Dementia (FTD) is a group of neurodegenerative disorders characterized by progressive damage to the frontal and temporal lobes of the brain, leading to changes in behavior, personality, and language abilities.
What are the common symptoms of FTD?
Common symptoms of FTD include changes in behavior (such as impulsivity, apathy, and disinhibition), language difficulties (including aphasia and apraxia), and cognitive decline (such as memory loss and executive dysfunction).
What causes Frontotemporal Dementia?
The exact cause of FTD is not fully understood, but it is believed to result from a combination of genetic, biological, and environmental factors. Certain genetic mutations have been linked to FTD, and a family history of the condition may increase the risk.
How is Frontotemporal Dementia diagnosed?

Diagnosing FTD typically involves a comprehensive evaluation, including a thorough medical history, physical examination, neuropsychological testing, and brain imaging studies (such as MRI or PET scans). Genetic testing may also be recommended in some cases.
Is there a cure for Frontotemporal Dementia?
Currently, there is no cure for FTD, but treatment options are available to help manage symptoms and improve quality of life. These may include medications to alleviate behavioral symptoms, speech therapy to address language difficulties, and supportive care to assist with daily activities. Ongoing research is focused on developing disease-modifying therapies and improving diagnostic techniques for FTD.

Understanding the Montreal Cognitive Assessment (MoCA) Test for Dementia
In this comprehensive guide, we explore the purpose, administration, interpretation, and significance of the Montreal Cognitive Assessment in the evaluation of dementia and cognitive impairment.