Source-Wiley-Online-Library
In the realm of neurodegenerative disorders, Posterior Cortical Atrophy (PCA) stands out as a rare and perplexing condition. While not as widely recognized as Alzheimer’s or Parkinson’s disease, PCA presents unique challenges due to its distinct pattern of brain degeneration and its profound impact on cognitive and visual functions. This article aims to delve into the intricacies of Posterior Cortical Atrophy, exploring its symptoms, causes, diagnostic approaches, and management strategies.
Understanding Posterior Cortical Atrophy
Posterior Cortical Atrophy, often referred to as “PCA,” is a neurodegenerative condition characterized by progressive degeneration of the posterior regions of the brain, particularly the occipital, parietal, and temporal lobes. Unlike typical Alzheimer’s disease, which primarily affects memory, PCA predominantly impairs visual processing, spatial awareness, and other higher-order visual functions. As a result, individuals with PCA may experience difficulties with reading, navigating space, recognizing faces, and perceiving objects accurately.
Unraveling the Symptoms of Posterior Cortical Atrophy
The symptoms of Posterior Cortical Atrophy can vary widely from person to person, reflecting the heterogeneous nature of the condition. However, common manifestations include:
- Visual disturbances: Patients often report blurred vision, difficulty focusing, and impaired depth perception.
- Visuospatial difficulties: Tasks that require orientation in space, such as driving or assembling puzzles, become challenging.
- Reading and writing impairments: Individuals may struggle to read text, write coherently, or comprehend written information.
- Object recognition problems: Recognizing faces, identifying familiar objects, and interpreting visual scenes may be compromised.
- Executive dysfunction: Difficulties with planning, organization, and problem-solving can arise as the disease progresses.
Exploring the Underlying Causes of Posterior Cortical Atrophy
The exact cause of Posterior Cortical Atrophy remains elusive, although it is often associated with underlying neurodegenerative conditions such as Alzheimer’s disease or dementia with Lewy bodies. In some cases, PCA may result from specific neurodegenerative proteinopathies, including tauopathies and synucleinopathies, which lead to the accumulation of abnormal proteins in the brain. Genetic factors may also play a role, as certain gene mutations have been implicated in familial forms of PCA.

The complexity of Posterior Cortical Atrophy (PCA) lies not only in its clinical manifestations but also in its underlying pathophysiology. While the exact cause of PCA remains elusive, researchers have made significant strides in understanding the diverse mechanisms that contribute to the development and progression of this neurodegenerative disorder.
One prominent hypothesis suggests that PCA often coexists with Alzheimer’s disease pathology, with a subset of individuals exhibiting a distinct pattern of cortical atrophy predominantly affecting the posterior brain regions. This association underscores the interconnectedness of neurodegenerative processes and highlights the need for further investigation into the underlying molecular pathways involved in PCA.
In addition to Alzheimer’s disease, PCA has been linked to other neurodegenerative proteinopathies characterized by the abnormal accumulation of specific proteins in the brain. Tauopathies, such as progressive supranuclear palsy (PSP) and corticobasal degeneration (CBD), are known to cause neurofibrillary tangles composed of hyperphosphorylated tau protein, which may contribute to the neurodegenerative changes observed in PCA.
Similarly, synucleinopathies, including dementia with Lewy bodies (DLB) and Parkinson’s disease dementia (PDD), involve the aggregation of alpha-synuclein protein, which can lead to neuronal dysfunction and degeneration in various brain regions, including the posterior cortex. The overlapping clinical and pathological features between PCA and these synucleinopathies further complicate the diagnostic process and highlight the need for biomarkers to distinguish between different neurodegenerative disorders accurately.
Genetic factors also play a role in the development of PCA, particularly in familial forms of the disease. Mutations in genes associated with Alzheimer’s disease, such as the amyloid precursor protein (APP), presenilin 1 (PSEN1), and presenilin 2 (PSEN2) genes, have been implicated in familial PCA cases. Additionally, mutations in other genes, such as GRN (progranulin) and MAPT (microtubule-associated protein tau), have been linked to familial frontotemporal dementia (FTD) syndromes, which may present with clinical features overlapping with PCA.
In summary, the underlying causes of Posterior Cortical Atrophy are multifaceted, involving a complex interplay of genetic, molecular, and environmental factors. Further research into the pathophysiology of PCA is essential for developing targeted therapies and biomarkers that can improve diagnostic accuracy and facilitate early intervention in this challenging neurodegenerative condition.
Navigating the Diagnostic Challenges
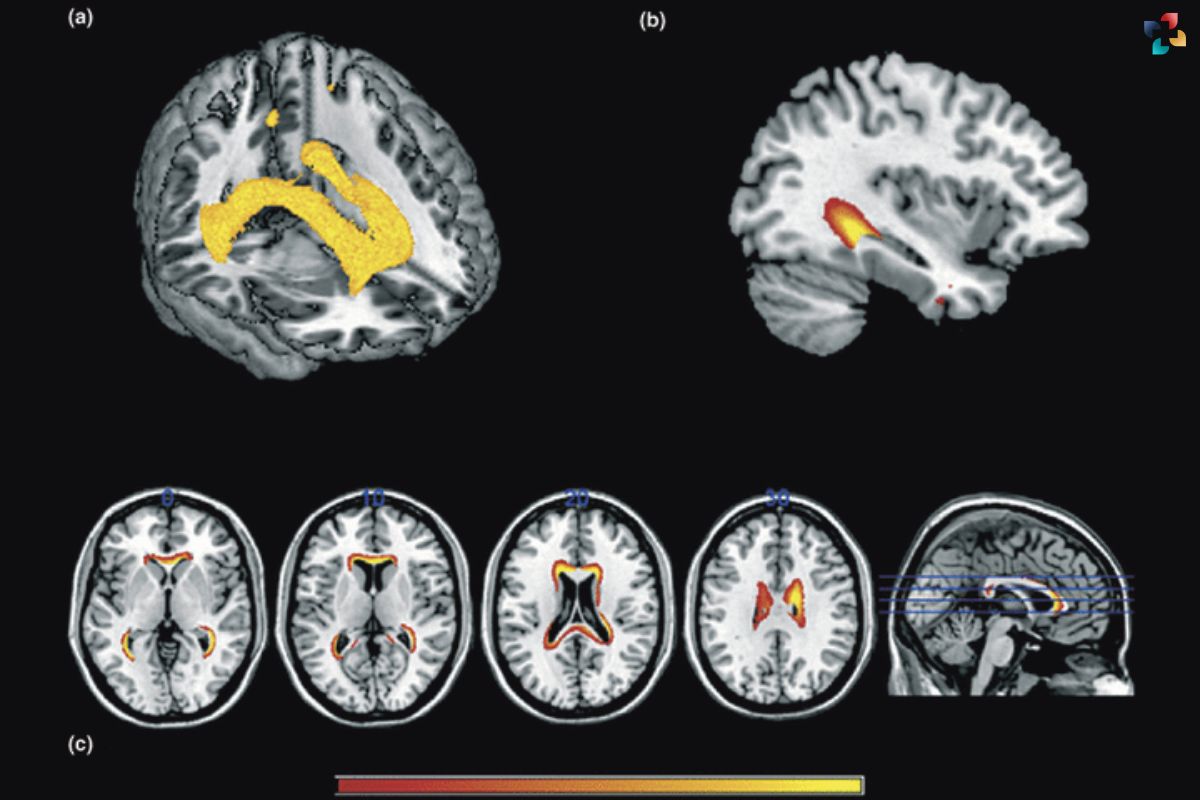
Diagnosing Posterior Cortical Atrophy can be challenging due to its atypical presentation and overlap with other neurodegenerative disorders. Comprehensive neurological and neuropsychological assessments are essential for identifying characteristic features of PCA, including visual-spatial deficits and disproportionate impairment of visual functions compared to memory. Advanced neuroimaging techniques, such as structural MRI and FDG-PET scans, can reveal patterns of cortical atrophy and hypometabolism in posterior brain regions, supporting the diagnosis of PCA.
Shedding Light on Management Strategies for Posterior Cortical Atrophy

While there is currently no cure for Posterior Cortical Atrophy, management strategies aim to alleviate symptoms, maximize functional independence, and enhance quality of life. Multidisciplinary approaches involving neurologists, ophthalmologists, neuropsychologists, and occupational therapists are crucial for providing comprehensive care to individuals with PCA. Treatment modalities may include:
- Visual aids and environmental modifications to accommodate visual impairments.
- Cognitive rehabilitation techniques to address memory and executive dysfunction.
- Pharmacological interventions to manage associated symptoms such as anxiety, depression, and sleep disturbances.
- Supportive services and caregiver education to assist families in coping with the challenges of PCA.
Conclusion: Navigating the Complexities of Posterior Cortical Atrophy
In conclusion, Posterior Cortical Atrophy remains a relatively obscure yet significant neurodegenerative condition, posing diagnostic and management challenges for clinicians and caregivers alike. By understanding the unique symptoms, underlying causes, and diagnostic approaches associated with PCA, healthcare professionals can better support individuals affected by this debilitating disorder. Continued research efforts aimed at unraveling the pathophysiology of PCA and developing targeted therapies offer hope for improved outcomes and enhanced quality of life for patients living with this condition.
FAQs
1. What are the main symptoms of Posterior Cortical Atrophy (PCA)?
The primary symptoms of PCA include visual disturbances such as blurred vision and difficulty focusing, visuospatial difficulties, reading and writing impairments, object recognition problems, and executive dysfunction.
2. Is Posterior Cortical Atrophy the same as Alzheimer’s disease?
While PCA shares some similarities with Alzheimer’s disease, it is a distinct neurodegenerative disorder characterized by predominant degeneration of the posterior regions of the brain, particularly the occipital, parietal, and temporal lobes.
3. How is Posterior Cortical Atrophy diagnosed?
Diagnosis of PCA involves comprehensive neurological and neuropsychological assessments to identify characteristic symptoms and cognitive deficits. Advanced neuroimaging techniques, such as MRI and PET scans, can help visualize patterns of cortical atrophy and hypometabolism in posterior brain regions, supporting the diagnosis.
4. Is Posterior Cortical Atrophy hereditary?
While most cases of PCA are sporadic, occurring randomly without a known cause, familial forms of the disease have been reported, suggesting a genetic component. Mutations in genes associated with Alzheimer’s disease and other neurodegenerative disorders may contribute to familial PCA cases.
5. Can Posterior Cortical Atrophy be treated or cured?
Currently, there is no cure for PCA, and treatment focuses on managing symptoms and maximizing functional independence. Multidisciplinary approaches involving neurologists, ophthalmologists, and occupational therapists can help individuals with PCA cope with the challenges of the disease and improve their quality of life.