Regenerative medicine is an emerging and promising field that aims to repair, replace, or regenerate human cells, tissues, or organs to restore normal function. This can be done in several ways – using stem cell therapies to introduce functional cells into damaged tissue, using tissue engineering to regenerate tissues and organs, or modulating regenerative processes to activate and enhance the body’s innate healing abilities. Significant advancements have been made in regenerative medicine in recent years, leading to the development and commercialization of novel therapies. This article provides an overview of some of the key regenerative medicine therapies that are currently on the market or late-stage clinical trials.
Stem Cell Therapies
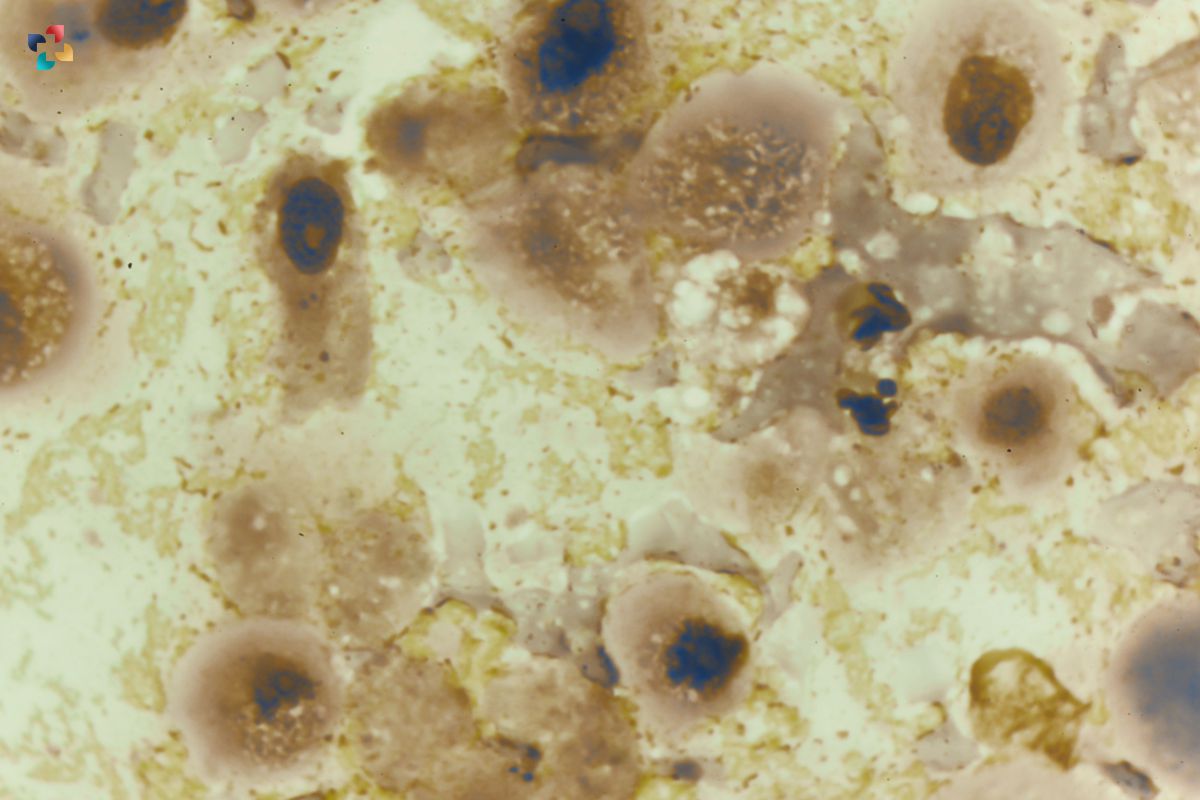
Stem cell therapies are one of the most widely explored approaches in regenerative medicine. These stem cell therapies involve introducing stem cells, which can give rise to many different cell types in the body, into damaged tissue to replace diseased or lost cells. Several stem cell-based products have been approved globally, such as Holoclar®, a limbal stem cell therapies for cornea regeneration, and various hematopoietic stem cell transplantation procedures for blood disorders. Adult stem cells derived from fat tissue and bone marrow are also being extensively studied in clinical trials for conditions such as myocardial infarction, autoimmune disorders, and neurological disorders.
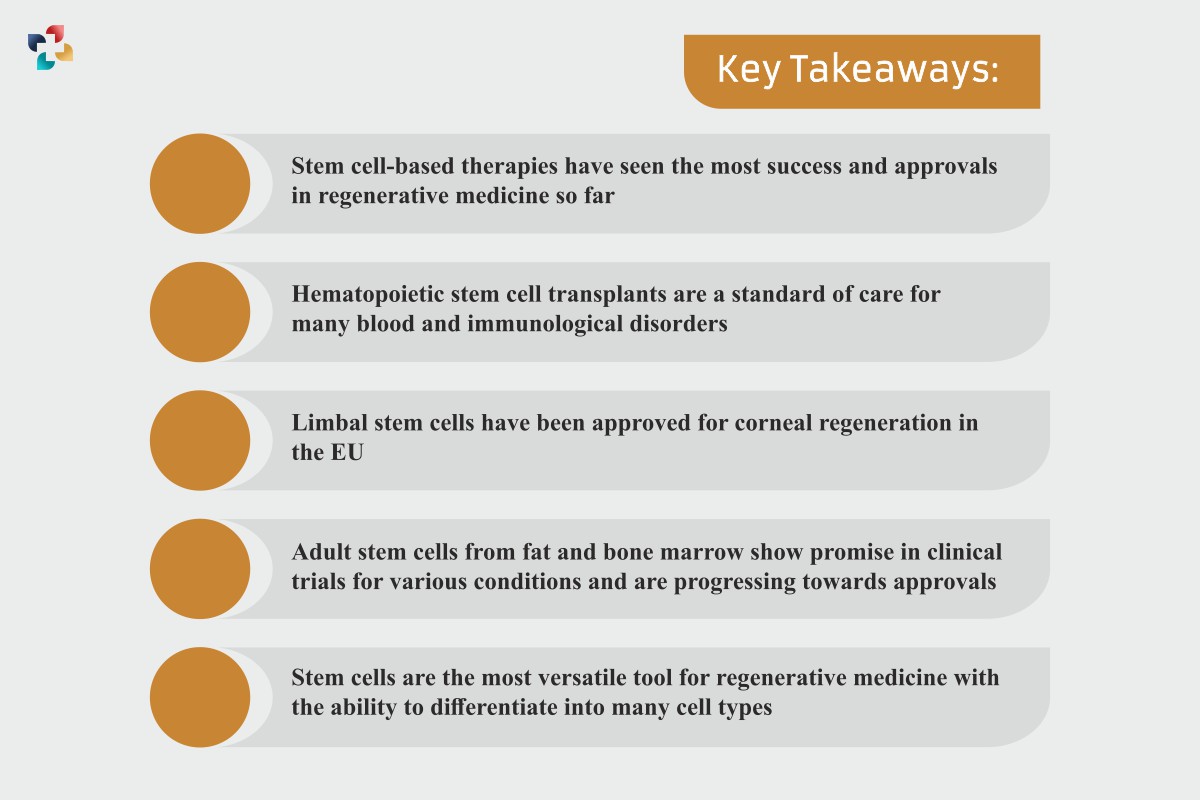
Key Takeaways:
- Stem cell therapies have seen the most success and approvals in regenerative medicine so far
- Hematopoietic stem cell transplants are a standard of care for many blood and immunological disorders
- Limbal stem cells have been approved for corneal regeneration in the EU
- Adult stem cells from fat and bone marrow show promise in clinical trials for various conditions and are progressing toward approvals
- Stem cells are the most versatile tool for regenerative medicine with the ability to differentiate into many cell types
Tissue-engineered Skin Products
Tissue engineering uses a combination of cells, engineering, and biomaterials to regenerate damaged tissues and organs. This field has seen significant clinical success in developing skin substitutes that provide functional, long-term skin tissue replacement. Epicel® and Integra® are two commercially available skin substitutes made by culturing skin cells on a biomaterial surface. These products are used for permanent skin tissue replacement in severe burn patients and chronic wounds. Other tissue-engineered skin products like Apligraf® and OrCelTM are also approved for the treatment of certain kinds of hard-to-heal wounds such as diabetic foot ulcers.
Key Takeaways:
- Tissue-engineered skin products are an approved regenerative therapy for burns and wounds
- Epicel and Integra are examples of commercially available permanent skin replacements
- Apligraf and OrCel promote healing of chronic wounds like diabetic foot ulcers
- Skin was one of the first commercial successes for tissue engineering and regenerative medicine
- Culturing a patient’s own skin cells on biomaterial scaffolds is a proven technique for skin regeneration
Platelet-rich Plasma
Platelet-rich plasma (PRP) is an emerging regenerative therapy that uses a patient’s own platelets from their blood as a source of growth factors and bioactive molecules to promote tissue healing and regeneration. PRP is produced by isolating and concentrating platelets from a blood sample. It contains an array of growth factors and cytokines that are actively secreted by the concentrated platelets to stimulate cellular migration, proliferation and angiogenesis – key processes in tissue regeneration. Several PRP preparation systems like Harvest Smart PRePTM and ArthrexAngel® are FDA-approved for creating PRP. PRP is being widely used for joint injuries, orthopaedic conditions like osteoarthritis, chronic wounds, bone regeneration, cosmetic procedures and more.
Key Takeaways:
- PRP leverages the body’s own healing mechanisms using patients’ platelets
- Multiple PRP preparation systems are approved for medical use
- PRP contains growth factors and cytokines that stimulate regeneration
- PRP is used in orthopaedics, wounds, bone regeneration and cosmetic procedures
- PRP provides a cost-effective and non-invasive regenerative treatment
Gene Therapies
Gene therapies deliver functional genes into cells to compensate for abnormal genes or provide a new function to the cell. These therapies harness the power of genetics to regenerate tissues by restoring protein production in tissues. Several regenerative gene therapies have been approved in recent years. Glybera® was the first approved gene therapy in the European Union in 2012 for lipoprotein lipase deficiency.
Luxturna®, approved by the FDA in 2017, uses a viral vector to deliver a normal copy of the RPE65 gene to correct vision loss due to an inherited retinal disease. Zolgensma® was approved in 2019 for spinal muscular atrophy, enabling babies and children with this neuromuscular disease to achieve developmental milestones. Gene therapies are poised to drive the next wave of innovation in regenerative medicine.
Key Takeaways:
- Gene therapies can restore normal genetic function and regenerate diseased tissues
- Luxturna, Zolgensma and Glybera are approved regenerative gene therapies
- Viral vectors are used to deliver healthy genes into patients’ cells
- Gene therapies are revolutionizing treatment for genetic diseases
- Correcting abnormal genes can lead to functional regeneration of tissues
- More gene therapies are in the pipeline for genetic disorders and cancers
Orthobiologics
Orthobiologics refer to biologically derived materials that orthopedic surgeons use to heal injuries, reduce inflammation, and promote tissue repair. These include substances made from human blood and plasma components or purified from other biological sources. Several ortho biologics products are approved as devices or biologics for bone, tendon, and cartilage regeneration. For example, Augment Bone Graft and Trinity Evolution Matrix comprise of bone morphogenetic protein and viable bone matrix approved as bone graft substitutes. Orthovisc® and Euflexxa® provide a hyaluronic acid composition to mimic synovial fluid and restore joint lubrication. Bioventus’ Exogen system uses low-intensity pulsed ultrasound to stimulate bone fractures to heal faster. These diverse ortho biologics promote musculoskeletal tissue healing through regeneration rather than just repair.
Key Takeaways:
- Orthobiologics stimulate the healing and regeneration of musculoskeletal tissues
- Products contain growth factors, proteins, living cells, or biomaterials
- Augment, Trinity Matrix, and Exogen are approved ortho-biologics
- Hyaluronic acid injections provide joint lubrication
- Orthobiologics promote regenerative healing for injuries, arthritis
- These can reduce the need for surgery or joint replacement
3D Bioprinting
3D bioprinting has emerged as an extension of 3D printing technology to generate functional three-dimensional tissues and organs from biological cell sources and biomaterials. With the ability to precisely position cells and biocompatible materials with supporting architecture, 3D bioprinting can recreate complex cellular interactions and tissue microenvironments. Although still largely experimental, viable 3D printed tissue constructs have been implanted in animal models for regeneration of bladder, skin, cartilage, bone and vascular tissues. A few startups like Organovo and Cyfuse Biomedical are moving towards commercializing 3D bioprinted tissues for human applications. Skin, bone and liver 3D bioprinted models are also being developed for clinical diagnostics and toxicity testing in the pharmaceutical industry.
Key Takeaways:
- 3D bioprinting enables positioning cells and biomaterials with precision
- It allows recreation of tissue and organ complexity outside the human body
- Startups are moving towards commercial 3D bioprinted products
- Skin, bone, and cartilage bioprinted tissues show regeneration potential
- Bioprinted tissue models will improve drug testing and discovery
- 3D bioprinting will eventually provide functional lab-grown organ transplants
Conclusion
Regenerative medicine leverages diverse technological approaches that stimulate the body’s inherent capacity to heal and regenerate. As discussed in this article, various stem cell therapies, tissue engineering methods, ortho biologics, early gene therapies, and 3D bioprinting have reached commercialization to make regenerative treatments a practical reality for today’s patients. Continuous progress in understanding mechanisms of tissue regeneration and innovations in enabling technologies will expand the promise of regenerative therapies for diverse degenerative diseases and unmet medical needs. While most applications today are focused on wound healing, orthopaedics, and rare genetic diseases, regenerative medicine holds enormous promise to profoundly impact healthcare in the coming decades.

Understanding Electrophysiology: Exploring the Intricacies of Cellular Activity
Within the field of physiology, electrophysiology examines the electrical characteristics of biological tissues and cells. It explores the processes by which electrical impulses are produced and transmitted in living things.