A Brain-Bone Axis Study suggests depression and osteoporosis may be biologically connected through a two-way “brain-bone axis,” potentially reshaping treatment strategies for older adults by highlighting how hormones, stress pathways, and inflammation interact across organs.
Researchers Highlight Emerging Brain-Bone Axis
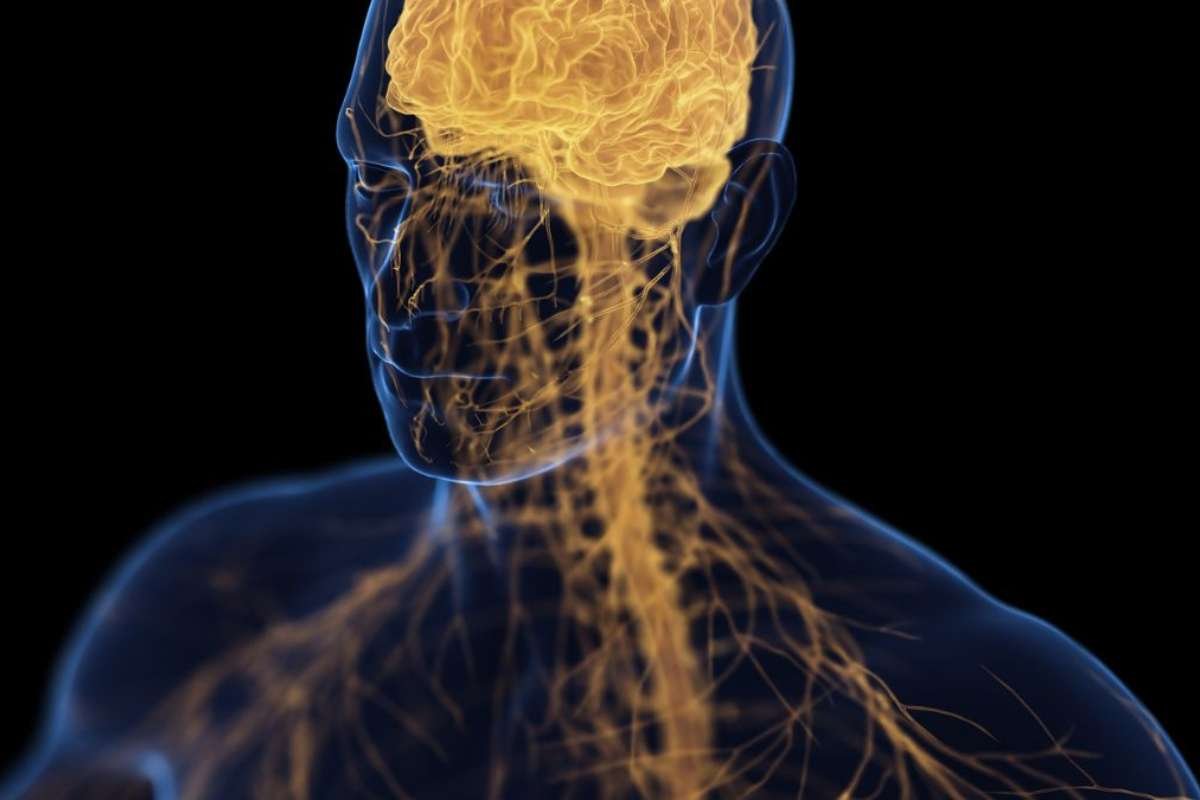
Neurologists in China report growing evidence that the brain and skeleton communicate through a physiological network once considered speculative. The review argues that recognizing this link could improve care for patients facing both mental and skeletal disorders.
“The clinical implications are substantial and immediate,” said authors Pengpeng Li of Xi’an Aerospace Hospital, Yangyang Gao of Ningxia Medical University, and Xudong Zhao of Jiangnan University. Their Brain-Bone Axis Study argues that “Clinicians across relevant specialties should recognize the interconnected pathophysiology of these conditions.”
Both depression and osteoporosis are common among older adults and frequently occur together. Research has shown that people with depression often experience reduced bone density, while those with osteoporosis tend to report higher rates of depression.
The authors propose that molecular and cellular mechanisms may unite the two conditions, with the brain-bone axis acting as a bridge.
Hormones and Proteins May Carry Signals Between Bone and Brain
Scientists increasingly view bones as hormone-producing organs capable of influencing distant systems, including the brain.
One hormone, osteocalcin, can cross the blood-brain barrier and affect cognitive function. Studies show acutely depressed patients have elevated osteocalcin levels that decline after treatment, suggesting a relationship with mood regulation.
Another bone-derived protein, osteopontin, appears to play an anti-inflammatory role in the brain and can remodel neurological tissue. According to a Brain-Bone Axis Study, Genetic variants tied to osteopontin production may also increase susceptibility to depression, according to the review.
The evolving understanding mirrors shifts in neuroscience and skeletal biology, where both organs are now seen as dynamic rather than fixed.
Stress Pathways Show Depression May Harm Bone Health
The relationship may work in reverse as well. Chronic activation of stress pathways in depression can trigger bone loss through brain-derived hormones such as cortisol and related inflammatory responses.
In effect, the severity of depression and osteoporosis may reinforce each other through shared biological processes, researchers said.
The team suggests future treatments could include customized exercise programs, neuromodulation, or medications targeting bone-derived signals that influence both mood and bone strength.
“Future investigations must validate axis-targeted interventions through rigorous clinical trials, but the current knowledge already supports incorporating this conceptual framework into patient management strategies,” the authors wrote, Brain-Bone Axis Study. They added that acknowledging the connection could help improve outcomes for vulnerable populations.
Source: https://www.sciencealert.com/brain-bone-axis-may-link-depression-with-osteoporosis-study-claims