Introduction:
Ulcerative colitis and Crohn’s disease are two types of inflammatory bowel diseases (IBD) that affect millions of people worldwide. While they share some similarities in symptoms and treatment, they also have distinct characteristics that differentiate them. In this article, we will delve into the key differences between ulcerative colitis and Crohn’s disease, including their symptoms, causes, diagnosis, and treatment options.
| Aspect | Ulcerative Colitis | Crohn’s Disease |
|---|---|---|
| Location of Inflammation | Primarily affects the colon and rectum. | Can affect any part of the digestive tract, including the |
| mouth, esophagus, stomach, small intestine, and colon. | ||
| Pattern of Inflammation | Inflammation typically starts in the rectum and may | Inflammation can occur in patches throughout the digestive |
| extend continuously up the colon in a uniform pattern. | tract and can be patchy, affecting segments of tissue. | |
| Symptoms | Abdominal pain, diarrhea (often bloody), rectal bleeding, | Abdominal pain, diarrhea (sometimes bloody), weight loss, |
| urgency to have a bowel movement. | fatigue, loss of appetite, fever. | |
| Complications | Increased risk of colon cancer, severe bleeding, | Increased risk of intestinal blockage (obstruction), |
| perforation of the colon, toxic megacolon (life-threatening | fistulas (abnormal connections between organs), strictures | |
| condition requiring immediate medical attention). | (narrowing of the intestines), malnutrition, intestinal | |
| abscesses. | ||
| Diagnosis | Combination of medical history evaluation, physical | Similar diagnostic tests as ulcerative colitis, including |
| examination, laboratory tests, imaging studies, and colonoscopy | blood tests, stool tests, colonoscopy with biopsy, imaging | |
| with biopsy. | studies. | |
| Treatment Options | Medications such as anti-inflammatory drugs, | Similar medications as ulcerative colitis, including |
| immunosuppressants, and biologic therapies. Surgery may | anti-inflammatory drugs, immunosuppressants, and biologic | |
| be necessary in severe cases to remove the colon (colectomy) | therapies. Surgery may involve removing affected parts of the intestines or creating an ostomy |
This table provides a concise overview of the key differences between ulcerative colitis and Crohn’s disease, including the location and pattern of inflammation, symptoms, complications, diagnosis, and treatment options for each condition. It serves as a useful reference tool for individuals seeking to understand the distinctions between these two types of inflammatory bowel diseases.
Understanding Ulcerative Colitis:
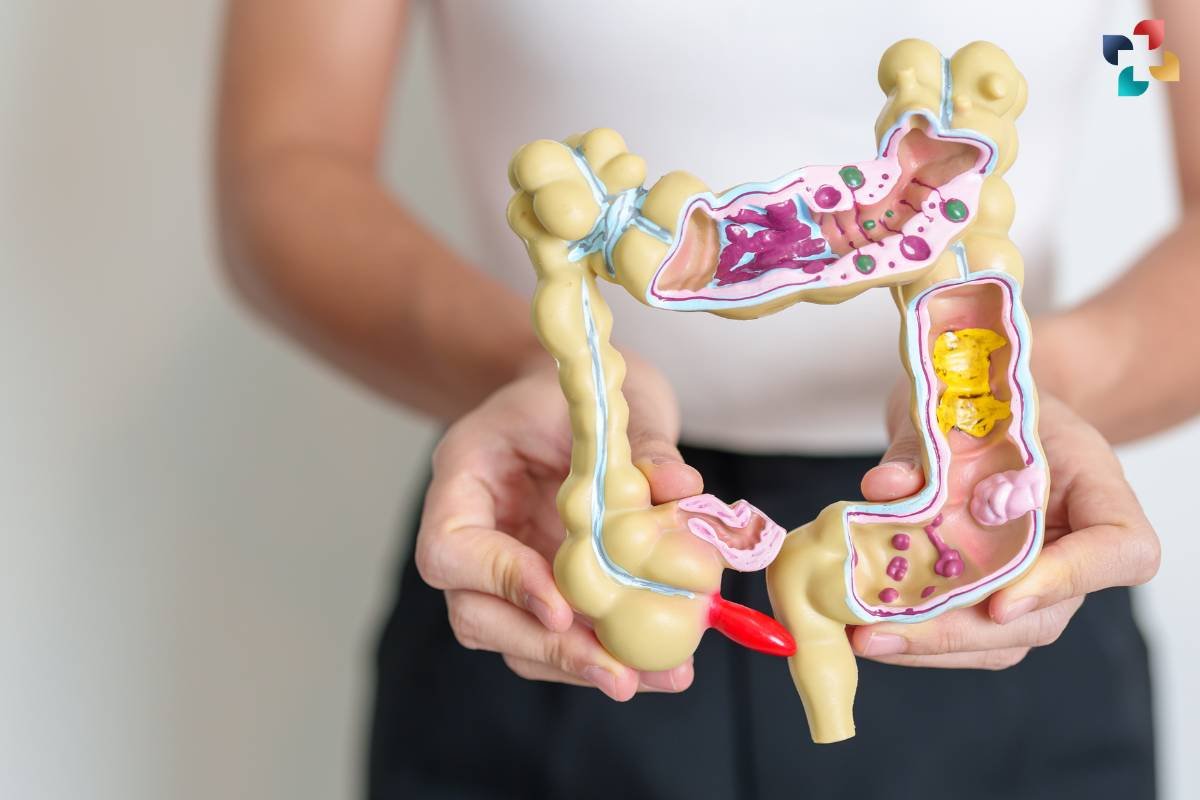
Ulcerative colitis is a chronic inflammatory condition that primarily affects the colon and rectum. It is characterized by inflammation and ulceration of the inner lining of the colon, leading to symptoms such as abdominal pain, diarrhea, rectal bleeding, and urgency to have a bowel movement. The inflammation in ulcerative colitis typically begins in the rectum and may extend continuously up the colon in a uniform pattern.
Causes and Risk Factors:
The exact cause of ulcerative colitis is unknown, but it is believed to involve a combination of genetic, environmental, and immune system factors. Family history of the disease, certain genetic predispositions, and environmental triggers such as stress, diet, and smoking may increase the risk of developing ulcerative colitis.
Diagnosis and Evaluation:
Diagnosing ulcerative colitis involves a combination of medical history evaluation, physical examination, laboratory tests, and imaging studies. Common diagnostic tests include blood tests to check for inflammation and anemia, stool tests to rule out infections, colonoscopy with biopsy to visualize the colon and obtain tissue samples for analysis, and imaging studies such as CT scans or MRIs to assess the extent of inflammation.
Treatment Options:
The goal of treatment for ulcerative colitis is to induce and maintain remission, alleviate symptoms, and improve quality of life. Treatment options may include medications such as anti-inflammatory drugs, immunosuppressants, and biologic therapies to reduce inflammation and modulate the immune response. In cases of severe or refractory disease, surgery to remove the colon (colectomy) may be necessary to alleviate symptoms and prevent complications.
Understanding Crohn’s Disease:

Crohn’s disease is a chronic inflammatory condition that can affect any part of the gastrointestinal tract, from the mouth to the anus. Unlike ulcerative colitis, which primarily affects the colon and rectum, Crohn’s disease can involve any layer of the intestinal wall and may occur in patches throughout the digestive tract.
Causes and Risk Factors:
Similar to ulcerative colitis, the exact cause of Crohn’s disease remains unclear, but it is thought to involve a combination of genetic, environmental, and immune factors. Family history of the disease, smoking, certain dietary factors, and alterations in the gut microbiome may increase the risk of developing Crohn’s disease.
Diagnosis and Evaluation:
Diagnosing Crohn’s disease also involves a combination of medical history evaluation, physical examination, laboratory tests, and imaging studies. Common diagnostic tests include blood tests, stool tests, colonoscopy, endoscopy, and imaging studies such as CT scans or MRIs to assess inflammation and evaluate the extent and severity of disease involvement.
Treatment Options:

Treatment for Crohn’s disease aims to reduce inflammation, alleviate symptoms, and prevent complications. Similar to ulcerative colitis, treatment options may include medications such as anti-inflammatory drugs, immunosuppressants, and biologic therapies. In addition, dietary modifications, nutritional support, and lifestyle changes may also play a role in managing symptoms and maintaining remission.
Conclusion:
In summary, while ulcerative colitis and Crohn’s disease are both types of inflammatory bowel diseases that share some similarities, they also have distinct differences in terms of symptoms, affected areas of the gastrointestinal tract, and treatment approaches. It is essential for individuals with these conditions to work closely with their healthcare providers to develop personalized treatment plans tailored to their specific needs and goals. By understanding the differences between ulcerative colitis and Crohn’s disease, patients can make informed decisions about their healthcare and better manage their condition for improved quality of life.
FAQs
1. What is ulcerative colitis?
Ulcerative colitis is a chronic inflammatory bowel disease that primarily affects the colon and rectum. It causes inflammation and ulcers in the lining of the large intestine, leading to symptoms such as abdominal pain, diarrhea, and rectal bleeding.
2. What are the common symptoms of ulcerative colitis?
Common symptoms of ulcerative colitis include abdominal pain, diarrhea (often bloody), rectal bleeding, urgency to have a bowel movement, fatigue, and weight loss. Symptoms can vary in severity and may come and go in flare-ups.
3. How is ulcerative colitis diagnosed?
Diagnosis of ulcerative colitis typically involves a combination of medical history evaluation, physical examination, laboratory tests (such as blood tests and stool tests), imaging studies (such as X-rays or CT scans), and a colonoscopy with biopsy to examine the colon and rectum lining for signs of inflammation.
4. What are the treatment options for ulcerative colitis?
Treatment for ulcerative colitis aims to reduce inflammation, control symptoms, and induce and maintain remission. Medications such as anti-inflammatory drugs, immunosuppressants, and biologic therapies are commonly used. In severe cases or if complications arise, surgery to remove the colon (colectomy) may be necessary.
5. What complications can arise from ulcerative colitis?
Complications of ulcerative colitis may include an increased risk of colon cancer, severe bleeding, perforation of the colon, toxic megacolon (a life-threatening condition requiring immediate medical attention), and the development of extraintestinal complications such as arthritis, skin problems, and liver disorders. Regular monitoring and management are essential to prevent and address complications.






