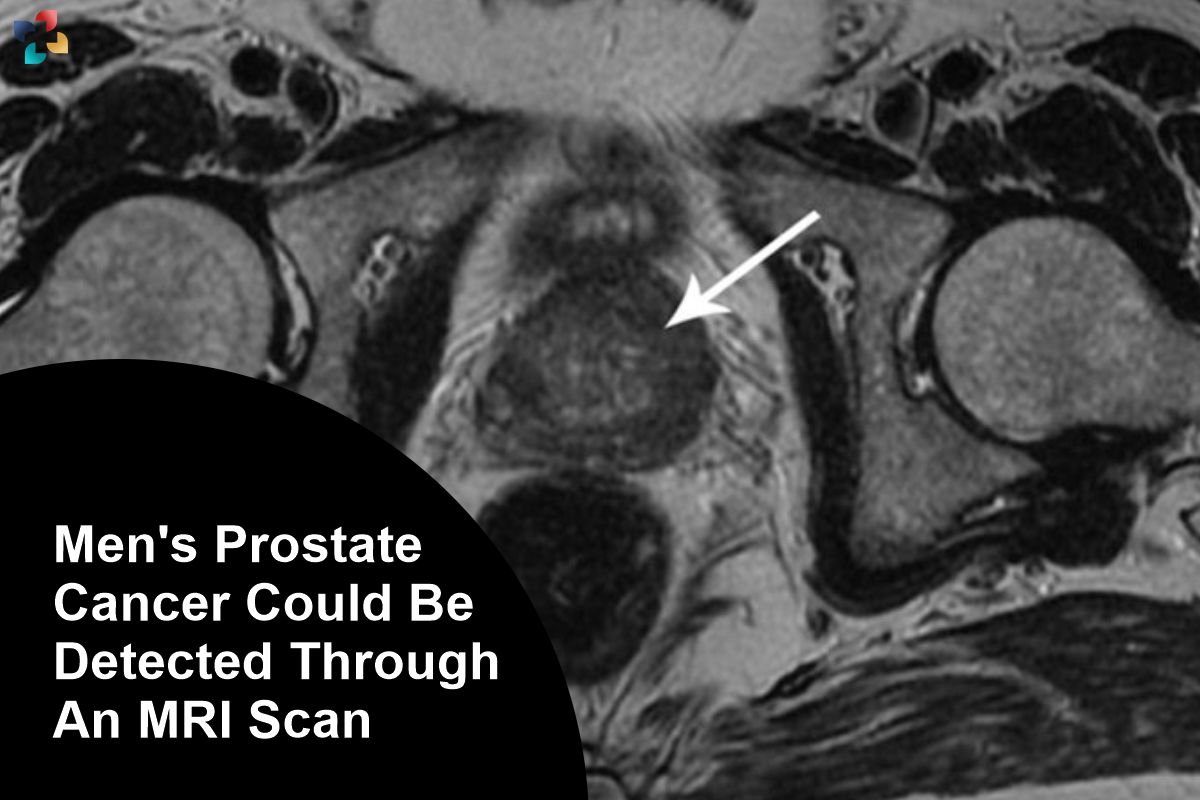
A new study suggests that men could be screened for prostate cancer with a 10-minute MRI scan. Blood tests, which check for elevated levels of a protein called PSA, showed to be much less effective at detecting cancer than the scans. Serious tumours that would not have been detected by PSA alone were discovered by MRI. Men over 50 can request a PSA test, but there is currently no universal screening system because PSA is thought to be too inaccurate.
Prostate cancer: what is it?
The prostate gland, which is a portion of the male reproductive system and is about the size of a walnut, is located in the pelvis beneath the bladder.
- It encircles the urethra, the tube that empties the body of pee through the penis.
- Aberrant, uncontrolled cell development is cancer.
- But it typically progresses gradually in the prostate.
- For years, there can be no indications or symptoms.
- And while some people never have any issues as a result of it, in others, the cancer can be lethal and aggressive.
Early detection and treatment are essential
Men aged 50 to 75 from London were recruited to University College Hospital for screening MRI and PSA testing as part of the Reimagine trial, which was reported in BMJ Oncology.
48 of the 303 patients who underwent both tests and had a positive MRI for cancer received additional testing, including biopsies, which revealed that 25 of them had severe malignancy.
More over half of the men whose cancer was discovered by MRI had low PSA test results below the accepted limit of 3 ng/ml, leading them to believe they were disease-free.
“Our results give an early indication that MRI could offer a more reliable method of detecting potentially serious cancers early, with the added benefit that less than 1% of participants were “over-diagnosed” with low-risk disease,” said Prof. Caroline Moore, consultant urologist UCLH and study’s principal investigator.
Being enrolled in the trial led to the diagnosis of prostate cancer for Paul Rothwell, 62. He was successfully treated because it was discovered early. He considers it a blessing that his PSA test came back negative because it would have provided erroneous reassurance if it hadn’t been for his MRI.
The BBC quoted Paul, a man from Hertfordshire, as saying: “If I’d just had the blood test I would be carrying on life as normal walking around unaware that there was some sort of ticking time bomb inside me of a cancer slowly growing, and by the time I did find out, presumably it would have been much harder to treat and much more dangerous to me.”
Prostate cancer PSA testing are regarded as helpful but unreliable markers. High levels, which may be a sign of cancer, can also be brought on by a recent infection, strenuous activity, or sex. As the experiment shown, a low PSA value may miss cancer as a result, which can result in overdiagnosis of the disease.
Although they note that a larger study would be required to evaluate this, the study’s authors make the suggestion that prostate MRI may be utilised for screening. Despite having a higher risk of prostate cancer, black men were five times less likely than white men to volunteer for the trial’s screening.
“One in four black men will develop prostate cancer during their lifetime, which is double the rate of men from other ethnicities,” said Saran Green, another study author from King’s College London. Any national screening strategy must include methods to contact black men and urge more of them to volunteer for testing given this increased risk.
13 years ago, Errol McKellar, 66, of Essex, received a prostate cancer diagnosis. After receiving successful treatment, he went back to his job as a mechanic and started giving customers discounts if they had their partner’s or their own prostate tested. He now manages the Errol McKellar Foundation, a nonprofit organisation that works to increase awareness of prostate cancer and encourage more men to be tested.
“When they brought their car in, I’d ask the men, ‘When was the last time you had a service and MOT on yourself?’,” he said in an interview with the BBC.
The African-Caribbean community has a serious distrust in the medical system, which needs to be addressed. But there are two more factors that we notice crop up frequently: one is fear, and the other is ignorance. Regardless of whether you are black or white, prostate cancer will kill you if you ignore it when it knocks on your door. In the end, it comes down to leaving no one behind.
A screening plan might be implemented within the next ten years, according to senior author Prof. Mark Emberton: “Due to our low levels of testing, the mortality rate for prostate cancer in the UK is double that of the US or Spain. I am certain that a national screening programme will considerably lower the prostate cancer mortality rate in the UK because prostate cancer is highly curable when discovered early.
“When a man’s prostate cancer is caught early, it’s very treatable,” said Simon Grieveson, Prostate Cancer UK’s assistant director of research. Sadly, more than 10,000 men get their cancer diagnosis after it has already spread.
“Research on how we might use these scans even more efficiently is wonderful to see. MRI images have altered the way we diagnose prostate cancer. We now want to see much larger, UK-wide studies to determine whether employing an MRI as the initial stage in testing may serve as the foundation for a national screening strategy because these results are so promising.
What signs should individuals look out for?
Common examples include:
- Trouble starting to urinate,
- Poor flow, and it takes a long time.
- Needing to urinate more frequently, especially at night.
- Blood in the urine or semen.
Other illnesses can also cause these symptoms, so it’s vital to have any changes examined by a specialist.