Nearly 1 in 5 emergency room visits worldwide are linked to abdominal pain, and a large portion of those cases start in the lower abdomen.
What often begins as a dull ache, mild cramp, or sudden twinge is one of the most common reasons people delay seeking medical advice. Many assume it’s caused by something minor, like indigestion or stress. In reality, ignoring early warning signs can allow serious conditions to quietly worsen.
The lower abdomen contains vital organs tied to digestion, urinary health, and reproduction. Pain in this area can range from harmless and short-lived to a red flag for infections, inflammation, or urgent medical emergencies.
This blog takes a clear, evidence-based look at lower abdominal pain, breaking down the most common causes, symptom patterns doctors rely on, and the key differences between mild discomfort and medical urgency. By the end, you’ll be better equipped to recognize signals early, reduce risk, and make informed decisions about your health without panic or guesswork.
What is Lower Abdominal Pain?
Pain in the lower abdomen below the belly button and above the pelvic area can signal issues with key organs involved in digestion, urination, or reproduction. Because multiple organs are packed in this small region, similar symptoms can have very different causes, making it one of the most common reasons people seek medical care.
Doctors divide the lower abdomen into three main areas to better understand what might be causing the pain:
- Lower right side – often linked to the appendix, intestines, or reproductive organs.
- Lower left side – commonly related to the colon and digestive system
- Center (just above the pelvis) – usually connected to the bladder and reproductive organs.
Studies show that clearly identifying the location of pain helps doctors make faster and more accurate decisions.
Types of Pain and What They Mean?
Not all pain feels the same, and that difference matters. Lower abdominal pain can feel like:
- Sharp pain, which may appear suddenly and needs quick attention
- Dull or aching pain, often linked to ongoing or mild issues.
- Cramping is commonly related to bowel changes or menstrual cycles.
- On-and-off pain, which may worsen after eating, physical activity, or stress
Doctors look at these pain patterns along with other symptoms to decide whether the issue is temporary or needs medical care.
Why Your Lower Abdomen Hurts?
Pain in the lower abdomen is a warning. In fact, clinical data show that digestive, urinary, and reproductive issues together account for over 70% of non-traumatic abdominal pain cases seen by doctors. What matters most is which system is sending the signal and how the pain behaves over time.
Understanding these causes can help you spot patterns early and avoid unnecessary panic or dangerous delays.
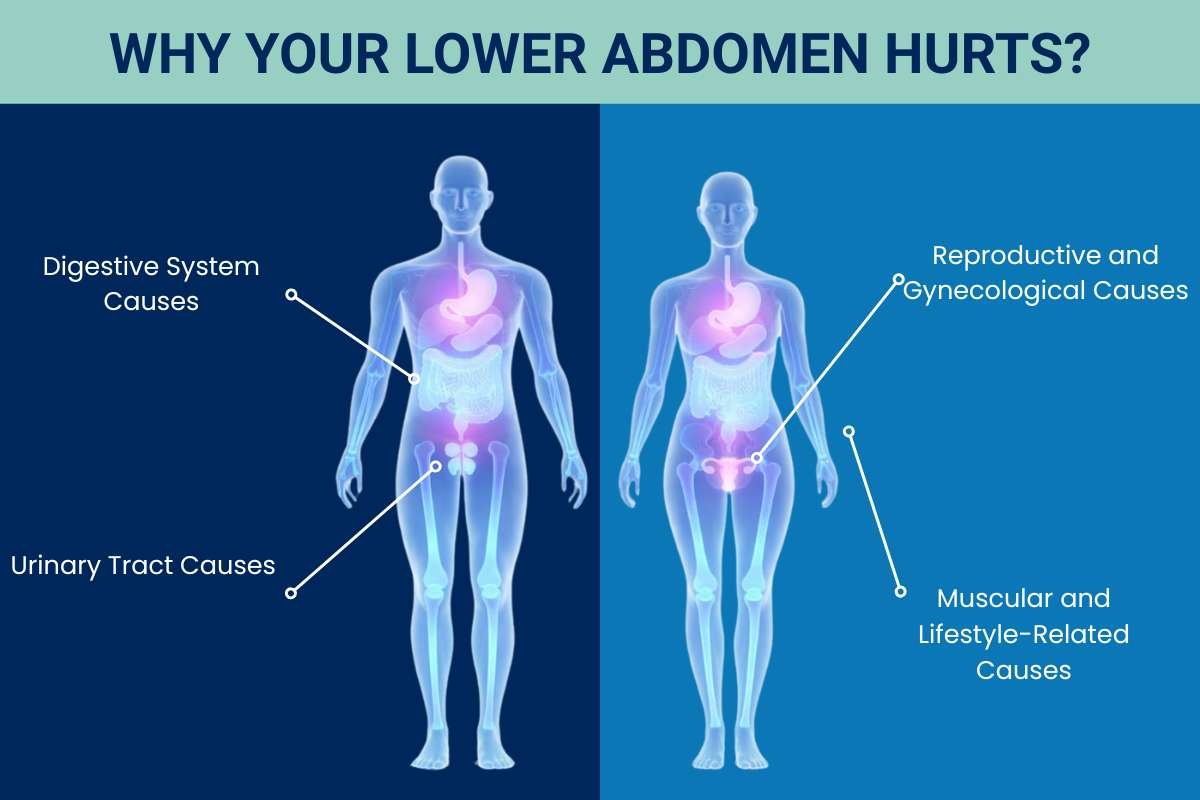
1. Digestive System Causes
Digestive problems are the leading cause of pain in the lower abdomen. According to gastroenterology studies, bowel-related issues explain nearly half of all recurring abdominal pain cases.
- Gas and constipation: One of the most common triggers. When stool moves slowly, pressure builds up, leading to bloating and cramping.
- Irritable Bowel Syndrome (IBS): A long-term condition affecting an estimated 10–23% of adults worldwide, often causing cramping, bloating, and unpredictable bowel habits.
- Appendicitis: Typically begins as mild discomfort and quickly turns into sharp pain on the lower right side. Delayed treatment can lead to serious complications.
- Diverticulitis: Inflammation of small pouches in the colon, more common after age 40, often causing left-sided pain and fever.
Digestive causes are often linked to diet, stress, and hydration, making lifestyle changes an important part of prevention.
2. Urinary Tract Causes
Urinary conditions are another major contributor, especially in adults.
- Urinary tract infections (UTIs) are one of the most common bacterial infections worldwide. Research shows that between 50% and 60% of women experience at least one UTI in their lifetime, often causing pressure and pain in the lower abdomen.
- Kidney stones: Known for causing intense, wave-like pain that can travel from the back to the lower abdomen.
- Bladder inflammation: Can lead to persistent discomfort in the center of the lower abdomen, often mistaken for digestive pain.
Urinary-related lower abdominal pain often comes with burning sensations, urgency, or changes in urine color.
3. Reproductive and Gynecological Causes
In women, reproductive organs play a significant role in pain patterns.
- Menstrual cramps: Affect up to 80% of women at some point and are usually harmless, though sometimes severe.
- Ovarian cysts: Often silent but can cause sharp, one-sided pain if they grow or rupture.
- Endometriosis: A chronic condition affecting around 1 in 10 women, known for causing recurring and sometimes severe pain.
- Early pregnancy-related changes: Mild discomfort can be normal, but sudden pain needs medical attention.
These causes often follow a monthly or hormonal pattern, which helps doctors identify them quickly.
4. Muscular and Lifestyle-Related Causes
Not all pain comes from internal organs, and this surprises many people.
- Muscle strain from workouts or heavy lifting
- Long hours of sitting, especially with poor posture
- Weak core muscles, leading to repeated discomfort
Muscular pain usually worsens with movement and improves with rest,t an important clue when evaluating lower abdominal pain.
Symptoms That Help Identify the Cause of the Pain
Rarely does lower abdomen discomfort show no symptoms. Your body usually sends supporting signals alongside the pain, small changes that can reveal a lot about what’s happening internally. Medical research shows that when doctors consider pain together with associated symptoms, they can narrow down the cause much faster and more accurately. That’s why paying attention to how your body feels as a whole is so important.
1. Pain With Digestive Changes
When lower abdominal pain is linked to digestion, it often develops gradually and changes throughout the day.
You may notice a feeling of fullness or bloating, even after eating small meals. Gas can build up, creating pressure that feels uncomfortable or cramp-like. Some people experience constipation, where bowel movements become less frequent, and stools feel hard to pass. Others may have diarrhea, especially during periods of stress or after certain foods.
Pain that worsens after meals or improves after using the bathroom is a strong sign that the digestive system is involved. These symptoms often fluctuate based on diet, hydration, and emotional stress, something doctors look for when identifying gut-related causes.
2. Pain With Urinary Symptoms
When the urinary system is involved, the pain often feels more like pressure or a constant ache in the center of the lower abdomen.
You might feel the need to urinate more often, even when very little urine comes out. There may be a burning or stinging sensation during urination, along with discomfort that doesn’t fully go away afterward. Changes in urine, such as cloudiness, a strong odor, or a darker color, are also common signs.
Urinary tract infections are among the most frequently diagnosed infections worldwide, and many people first notice them because of lower abdominal discomfort rather than urinary symptoms alone.
3. Pain With Fever, Nausea, or Extreme Fatigue
When pain is paired with symptoms like fever, nausea, or unusual tiredness, it often means the body is fighting inflammation or infection.
A fever suggests the immune system is actively responding to a problem. Nausea or vomiting may appear when the digestive system becomes irritated or when inflammation spreads. Some people also feel suddenly drained or weak, even without physical activity.
When lower abdominal pain comes with these symptoms, especially if the pain becomes sharper or more intense,e doctors treat it as a warning sign that should not be ignored.
4. Pain Patterns That Raise Immediate Concern
Certain pain behaviors stand out as more serious:
- Pain that appears suddenly and intensifies quickly
- Pain that wakes you from sleep
- Pain that keeps worsening instead of easing
- Pain accompanied by blood in urine or stool
These patterns often indicate conditions that need prompt medical evaluation rather than home remedies or waiting it out.
Read Next:
- Know What Hurts You Most with Abdominal Quadrants and Organs?
- Recognizing the Signs of Appendicitis: A Comprehensive Guide
Lower Abdominal Pain in Men vs Women: Key Differences
Men and women experience lower abdomen discomfort in different ways because of differences in anatomy and hormones. Understanding these differences helps identify causes faster and prevents misdiagnosis.
Why Causes Differ?
- Women: Pain is often linked to reproductive organs and hormonal cycles. Conditions like menstrual cramps, ovulation pain, ovarian cysts, and endometriosis are unique to women. Digestive and urinary issues also occur, but may overlap with reproductive symptoms.
- Men: Pain is more commonly associated with urinary or muscular issues, like kidney stones, urinary tract infections, prostate problems, or muscle strain. Reproductive-related causes are less frequent but may include testicular or prostate-related pain.
Table Showing Comparison of Lower Abdominal Pain in Men vs Women
| Aspect | Women | Men | Data |
| Most Common Causes | Menstrual cramps, ovulation pain, ovarian cysts, endometriosis, UTIs, digestive issues | Kidney stones, UTIs, prostate problems, digestive issues, muscle strain | Women report 60–70% of chronic lower abdominal pain cases; endometriosis affects 10% reproductive age women worldwide |
| Pain Pattern | Often cyclical with the menstrual cycle; can be crampy, dull, or sharp | Often constant or triggered by activity; can be sharp or aching | Pattern helps doctors narrow down reproductive vs urinary/muscle causes |
| Associated Symptoms | Bloating, nausea, irregular periods, pelvic pressure, fatigue | Urgency or burning during urination, back pain, pressure, and cramps after physical exertion | Symptom clusters are critical for early diagnosis |
| Red Flags | Sudden sharp pain, fever, abnormal bleeding, pain unrelieved by rest | Sudden severe pain, fever, blood in urine, worsening pain with activity | Immediate medical evaluation is recommended for these signs |
| Prevalence | Up to 80% experience menstrual cramps; UTIs affect ~50% of women at least once | UTIs less frequent; kidney stones affect ~12% of men | Digestive and urinary issues affect both sexes, but prevalence varies |
10 Common Reasons Your Lower Abdomen May Hurt
1. Gas & Constipation
| Symptoms | Bloating, cramping, irregular stools |
| Pain Location | Central/lower abdomen |
Gas and constipation are among the most common, usually minor, causes of lower abdominal discomfort. They often result from diet, hydration, or irregular bowel habits, and while usually not serious, they can still cause noticeable bloating and cramps.
- Can worsen after eating certain foods like beans, cabbage, or carbonated drinks
- Often relieved by mild exercise or abdominal massage
- Chronic constipation may lead to hemorrhoids or discomfort during bowel movements
2. Irritable Bowel Syndrome (IBS)

| Symptoms | Cramping, diarrhea, or constipation, bloating |
| Pain Location | Lower abdomen, often diffuse |
IBS is a chronic digestive disorder that causes recurring lower abdominal pain, bloating, and changes in bowel habits. Stress, diet, and gut sensitivity all play a role.
- Pain often improves after bowel movements but returns later
- Trigger foods can vary widely between individuals
- Stress management and dietary adjustments can reduce symptom frequency
3. Appendicitis
| Symptoms | Sudden sharp pain, nausea, and fever |
| Pain Location | Lower right abdomen |
Appendicitis occurs when the appendix becomes inflamed. It usually starts with mild discomfort that quickly intensifies and requires urgent medical attention.
- Pain may initially appear near the belly button before shifting to the lower right side.
- Loss of appetite and mild digestive upset are common early signs
- Untreated appendicitis can lead to rupture and serious complications
4. Diverticulitis

| Symptoms | Left-sided pain, constipation or diarrhea, fever |
| Pain Location | Lower left abdomen |
Diverticulitis is the inflammation of small pouches in the colon, often causing pain on the lower left side. It typically affects middle-aged and older adults.
- May cause changes in bowel habits, alternating between constipation and diarrhea
- Can be triggered by low-fiber diets
- Recurrent episodes may require surgery in severe cases
5. Urinary Tract Infection (UTI)
| Symptoms | Burning during urination, urgency, cloudy urine, lower abdominal pressure |
| Pain Location | Central/lower abdomen |
UTIs occur when bacteria infect the urinary system. They can cause discomfort in the lower abdomen, burning sensations, and frequent urination.
- More common in women due to a shorter urethra
- Poor hygiene or holding urine for long periods increases the risk
- Untreated UTIs can progress to kidney infections
6. Kidney Stones

| Symptoms | Severe waves of pain, nausea, and blood in the urine |
| Pain Location | Lower back radiating to the lower abdomen |
Kidney stones are hard deposits of minerals that form in the kidneys. They can cause sudden, intense pain radiating to the lower abdomen.
- Pain often comes in waves and may move as the stone passes
- Dehydration is a major risk factor for stone formation
- Stones smaller than 5mm often pass naturally; larger ones may require intervention
7. Menstrual Cramps
| Symptoms | Cramping, bloating, fatigue |
| Pain Location | Lower abdomen, central or one-sided |
Menstrual cramps, or dysmenorrhea, affect most women during their periods, causing cramping, bloating, and fatigue.
- Pain is usually worse in the first 1–2 days of menstruation
- Exercise and heat therapy can help alleviate discomfort
- Severe cramps may indicate underlying conditions like fibroids
8. Ovarian Cysts

| Symptoms | Dull or sharp one-sided pain, bloating, nausea |
| Pain Location | Lower right or left abdomen |
Ovarian cysts are fluid-filled sacs on the ovary. They can cause dull or sharp lower abdominal pain, sometimes with bloating or nausea.
- Pain can increase during sexual activity or exercise
- Hormonal fluctuations can cause cyst growth or shrinkage
- Most cysts resolve on their own, but some require medical monitoring
9. Endometriosis
| Symptoms | Recurring cramps, bloating, fatigue |
| Pain Location | Lower abdomen, pelvic area |
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus. This leads to recurring lower abdominal pain and sometimes fatigue or bloating.
- Pain often worsens during menstruation or ovulation
- Can affect fertility if left untreated
- Early diagnosis improves management and quality of life
10. Muscle Strain / Injury
| Symptoms | Pain worsens with movement, tenderness |
| Pain Location | Lower abdomen, often sides |
Muscle strain or injury in the lower abdomen can occur from exercise, heavy lifting, or sudden movements.
- Pain usually worsens with movement or certain positions
- Strengthening core muscles can help prevent recurrence
- Ice, rest, and anti-inflammatory measures aid recovery
Read Next:
- Are You Ignoring the Signs of Irritable Bowel Syndrome Disease? Here’s What Your Gut’s Telling You
- Understanding Irritable Bowel Syndrome: Causes, Symptoms, and Management Strategies
When to See a Doctor for Lower Abdominal Pain?
Certain signs indicate a more serious underlying illness, even though many causes of lower abdomen discomfort are moderate and transient. Knowing when pain crosses the line from manageable to concerning can prevent complications and ensure timely treatment.
You should seek medical attention if you experience the pain:
- Persists for more than a few days despite home care
- Becomes progressively worse instead of improving
- Interferes with daily activities, sleep, or movement
1. Warning Signs That Require Immediate Medical Attention
Certain symptoms accompanying the pain indicate the need for urgent evaluation rather than watchful waiting.
Key Red Flags:
- Sudden, severe, or sharp pain that appears without warning
- Pain accompanied by high fever, chills, or persistent vomiting
- Blood in urine, stool, or abnormal vaginal bleeding
2. Pain Patterns That Deserve Closer Evaluation
The nature and behavior of pain often provide important diagnostic clues and should not be overlooked.
Important Observations:
- Pain that shifts location may indicate organ involvement
- Pain that worsens with pressure or release can suggest inflammation
- Recurring pain following meals or bowel movements may point to digestive disorders
3. Special Considerations for Women
Lower abdominal discomfort in women can sometimes be linked to reproductive health, making timely assessment particularly important.
Situations to Watch For:
- Pain associated with missed periods or suspected pregnancy
- Severe menstrual pain that worsens over time
- Lower abdominal discomfort combined with pelvic pressure or pain during intercourse
How is Lower Abdominal Pain Diagnosed?
Because lower abdominal discomfort can come from many different organs, doctors follow a step-by-step diagnostic approach rather than relying on symptoms alone. This method reduces guesswork and ensures that serious conditions are not missed.
1. Medical History: The First Clue
Diagnosis often begins with detailed questions, as your answers can narrow down the cause quickly.
Doctors typically ask about:
- When the pain started, and whether it came on suddenly or gradually
- The exact location and type of pain (sharp, dull, cramping, or constant)
- Triggers such as eating, movement, urination, or menstrual cycles
Studies show that a thorough medical history alone can guide diagnosis in nearly 70% of abdominal pain cases, reducing unnecessary tests.
2. Physical Examination: Reading the Body’s Signals
A hands-on exam helps doctors understand how your body reacts to pressure and movement.
During the exam, they may check for:
- Tenderness or guarding in specific abdominal areas
- Swelling or abnormal masses
- Pain changes when muscles are tightened or released
These findings often help distinguish between digestive, urinary, or reproductive causes.
3. Diagnostic Tests and Imaging
When symptoms are unclear or severe, medical tests provide confirmation and clarity.
Common diagnostic tools include:
- Blood tests to detect infection, inflammation, or anemia
- Urine tests to identify urinary tract or kidney issues
- Ultrasound or CT scans to visualize organs and locate blockages, stones, or inflammation
Research indicates that imaging studies significantly improve diagnostic accuracy, especially when pain is localized or worsening.
Treatment Options for Lower Abdominal Pain
Treatment for lower abdominal discomfort depends entirely on the underlying cause. Some cases improve with simple lifestyle changes, while others require medication or medical procedures. The key is matching the treatment to the cause, not just treating the pain itself.
At-Home Care for Mild and Temporary Pain
Many mild cases of the pain can be managed safely at home, especially when symptoms are short-lived and not severe.
Helpful measures include:
- Resting and avoiding strenuous activity that may worsen discomfort
- Staying hydrated to support digestion and urinary health
- Using warm compresses or heating pads to relax muscles and reduce cramping
Studies suggest that heat therapy can significantly reduce abdominal muscle tension and improve comfort in non-emergency cases.
Medications Used for Symptom Relief
When pain persists or interferes with daily life, medications may be recommended based on the cause.
Common options include:
- Pain relievers to reduce inflammation and discomfort
- Antibiotics are used when bacterial infections are identified.
- Antispasmodics to ease intestinal or bladder spasms
Doctors avoid unnecessary medication and focus on targeted treatment to prevent side effects and recurrence.
Medical Procedures and Advanced Treatment
Some causes of the pain require medical intervention beyond medication.
Examples include:
- Procedures to remove blockages, stones, or inflamed tissue
- Surgical treatment in cases like appendicitis or severe gynecological conditions
- Hospital-based care when pain is severe, sudden, or accompanied by complications
Early treatment has been shown to lower recovery time and reduce the risk of long-term issues.
How to Prevent Lower Abdominal Pain?
While not all causes can be avoided, many cases of lower abdominal discomfort are linked to daily habits. Small, consistent lifestyle changes can significantly reduce how often pain occurs and how intense it feels.
1. Diet and Digestive Health
What you eat directly affects how your digestive system functions, making diet a key prevention factor.
Helpful habits include:
- Eating fiber-rich foods to support regular bowel movements
- Limiting processed foods that can trigger bloating and discomfort
- Eating smaller, balanced meals to reduce digestive strain
Research shows that balanced diets lower the risk of common digestive causes of lower abdominal pain, including constipation and gas-related discomfort.
2. Hydration and Urinary Health
Proper hydration plays a major role in preventing urinary and kidney-related pain.
Key practices:
- Drinking enough water throughout the day
- Avoiding excessive caffeine and sugary drinks
- Emptying the bladder regularly to prevent infections
Studies indicate that adequate hydration can reduce the risk of urinary tract infections, a frequent cause of lower abdominal discomfort.
3. Physical Activity and Core Health
Movement helps keep abdominal organs functioning smoothly.
Preventive steps include:
- Regular light exercise to improve digestion and circulation
- Gentle stretching to reduce muscle tension
- Avoiding prolonged sitting, which can worsen abdominal pressure
Even moderate daily activity has been shown to improve gut motility and reduce abdominal discomfort.
Read Next: Understanding Abdominal Quadrants: Anatomy, Function, and Clinical Significance
Common Myths About Lower Abdominal Discomfort
Despite how common lower abdominal discomfort is, many people misunderstand what it means or when it should be taken seriously. Clearing up these myths helps readers make safer, more informed decisions.
Myth 1: Lower Abdominal Pain Is Always Digestive
Many assume that stomach issues are the only cause, but this isn’t true.
- Pain can originate from the urinary or reproductive system
- Non-digestive causes account for a significant number of ER visits
- Treating it as “just gas” can delay proper care
Medical data shows that abdominal pain has multiple overlapping causes, which is why self-diagnosis can be risky.
Myth 2: Severe Pain Always Means a Serious Problem
Pain intensity alone doesn’t always reflect severity.
- Mild pain can sometimes signal chronic conditions
- Serious issues may begin with subtle discomfort
- Pain patterns matter more than pain level
Doctors focus on duration, location, and associated symptoms rather than intensity alone.
Myth 3: Pain Will Go Away on Its Own
Waiting too long can sometimes worsen outcomes.
- Some conditions progress quietly.
- Early treatment often shortens recovery time.
- Ignoring recurring pain increases complication risks.
Studies consistently show better outcomes when abdominal symptoms are evaluated early.
Conclusion
Lower abdominal pain is a common issue that can range from minor digestive discomfort to serious medical conditions. Understanding the underlying cause, associated symptoms, and risk factors is essential for effective management.
Most mild pain can be managed with healthy lifestyle choices, such as a balanced diet, hydration, regular exercise, and stress management. However, persistent, severe, or sudden pain, especially when accompanied by fever, vomiting, or blood, should never be ignored and requires prompt medical attention.
By paying attention to your body, recognizing warning signs, and seeking timely care when needed, you can reduce complications and improve overall well-being. Awareness, prevention, and informed action remain the most reliable ways to stay healthy and address lower abdominal discomfort effectively.
FAQs
1. What are the most common causes of lower abdominal pain?
Lower abdominal discomfort can arise from digestive issues like gas, constipation, or IBS, urinary problems such as UTIs or kidney stones, and, in women, reproductive conditions like menstrual cramps, ovarian cysts, or endometriosis. Understanding the accompanying symptoms helps identify the likely cause.
2. When should the pain be considered an emergency?
Pain is considered urgent if it is sudden, severe, or accompanied by fever, persistent vomiting, blood in urine or stool, or pain that worsens rapidly. Conditions like appendicitis, kidney stones, or infections require immediate medical attention.
3. Can lifestyle habits prevent lower abdominal discomfort?
Yes. Maintaining a fiber-rich diet, staying hydrated, exercising regularly, and managing stress can reduce the frequency and severity of many common causes of pain, such as constipation, IBS, or menstrual cramps.
4. Does age affect the causes of lower abdominal pain?
Absolutely. Younger adults often experience menstrual cramps, ovarian cysts, or IBS, while middle-aged and older adults are more prone to diverticulitis, kidney stones, or urinary tract infections. Recognizing age-related patterns can help in early detection.
5. How is lower abdominal discomfort diagnosed by doctors?
Doctors combine medical history, physical exams, and diagnostic tests such as blood tests, urine analysis, ultrasounds, or CT scans. This systematic approach helps identify whether the pain is digestive, urinary, reproductive, or muscular in origin.






