Source-Genetic-Engineering-and-Biotechnology-News
Creutzfeldt-Jakob Disease (CJD) is a rare, degenerative, and invariably fatal brain disorder that affects about one in every one million people worldwide annually. Despite its rarity, CJD poses significant challenges due to its rapid progression and devastating effects on the central nervous system. This article aims to provide a comprehensive overview of Creutzfeldt-Jakob Disease, including its causes, symptoms, diagnosis, and treatment options.
Creutzfeldt-Jakob Disease is classified into several subtypes, including sporadic, familial, iatrogenic, and variant CJD. Sporadic CJD, which occurs spontaneously without any known cause, is the most common form, accounting for about 85% of cases. Familial CJD is inherited, resulting from mutations in the PRNP gene, while iatrogenic CJD is acquired through medical procedures such as transplantation of infected tissues or exposure to contaminated surgical instruments. Variant CJD, on the other hand, is linked to the consumption of contaminated beef products containing abnormal prion proteins, primarily seen in countries affected by bovine spongiform encephalopathy (BSE), also known as “mad cow disease.”
Causes and Risk Factors
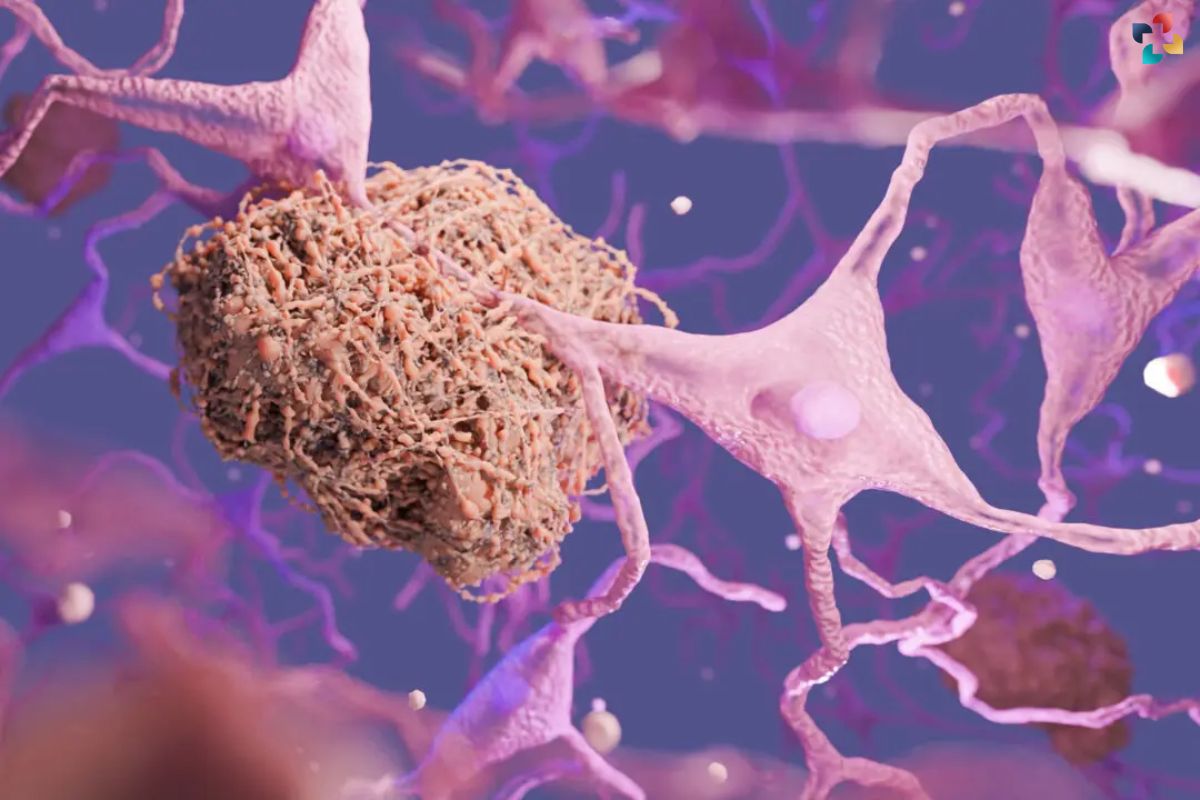
Creutzfeldt-Jakob Disease (CJD) is caused by the abnormal folding of prion proteins in the brain, leading to the formation of insoluble aggregates that damage nerve cells. While the exact mechanism behind this misfolding remains unclear, several factors have been associated with the development of CJD.
One of the primary risk factors for sporadic CJD, the most common form of the disease, is age, with the majority of cases occurring in individuals over the age of 60. However, sporadic CJD can affect people of any age, albeit less frequently. Certain genetic mutations in the PRNP gene have been linked to familial CJD, a rare inherited form of the disease. These mutations can alter the structure of prion proteins, increasing the likelihood of abnormal folding and aggregation.
Iatrogenic CJD can occur as a result of medical procedures that expose individuals to contaminated tissues or instruments containing infectious prions. This includes corneal transplants, dura mater grafts, and neurosurgical procedures involving contaminated equipment. Although stringent sterilization protocols have significantly reduced the risk of iatrogenic transmission, sporadic cases still occur occasionally.
Variant CJD, often referred to as “mad cow disease,” is believed to result from the consumption of beef products contaminated with prions from infected cattle. The outbreak of bovine spongiform encephalopathy (BSE) in the late 20th century raised concerns about the potential transmission of prion diseases to humans through the food chain. Variant CJD primarily affects younger individuals and is characterized by a distinct clinical and pathological profile compared to other forms of CJD.
Symptoms of Creutzfeldt-Jakob Disease typically manifest gradually and worsen over time. Cognitive impairment, including memory loss, confusion, and difficulty concentrating, is often among the initial symptoms experienced by affected individuals. As the disease progresses, patients may develop behavioral changes such as irritability, agitation, and mood swings. Motor symptoms such as muscle stiffness, tremors, and coordination problems may also become apparent, leading to difficulties with walking and mobility.
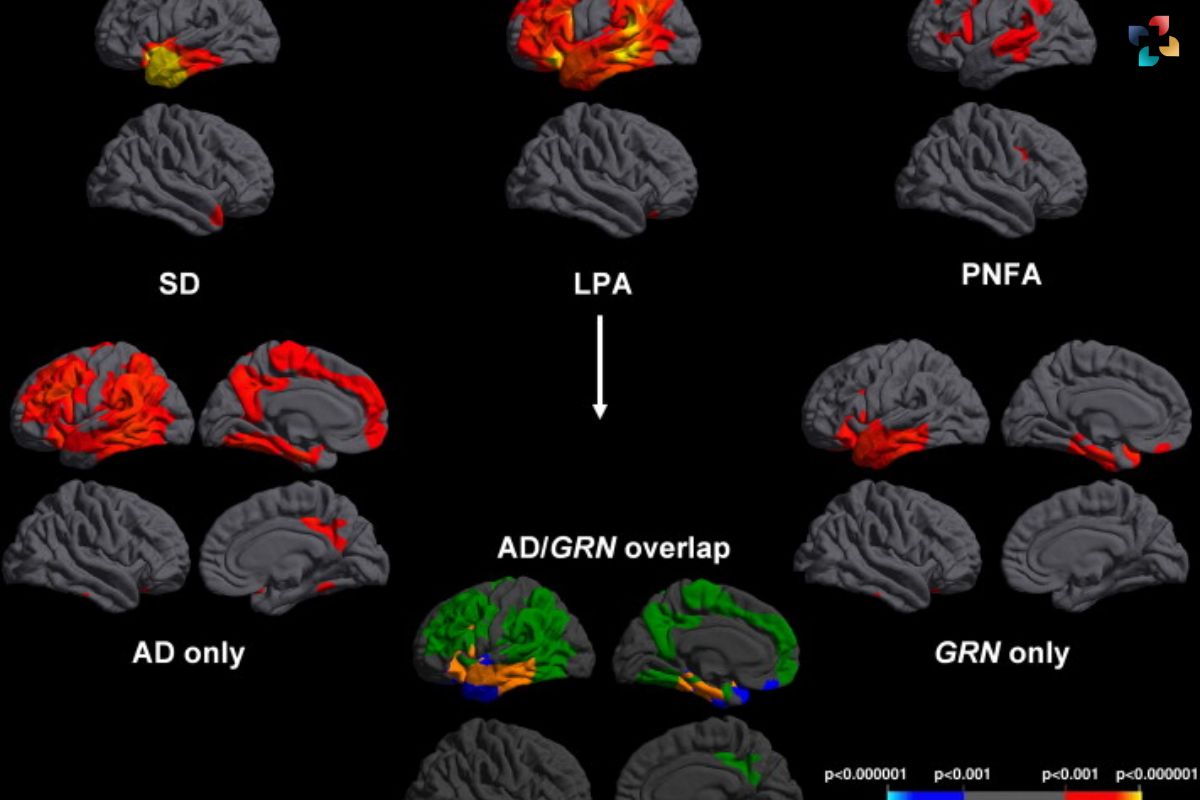
The rapid deterioration of neurological function sets CJD apart from other neurodegenerative disorders, such as Alzheimer’s disease and Parkinson’s disease, which tend to progress more slowly. This rapid decline in health underscores the urgency of accurate diagnosis and prompt intervention to provide supportive care and manage symptoms effectively.
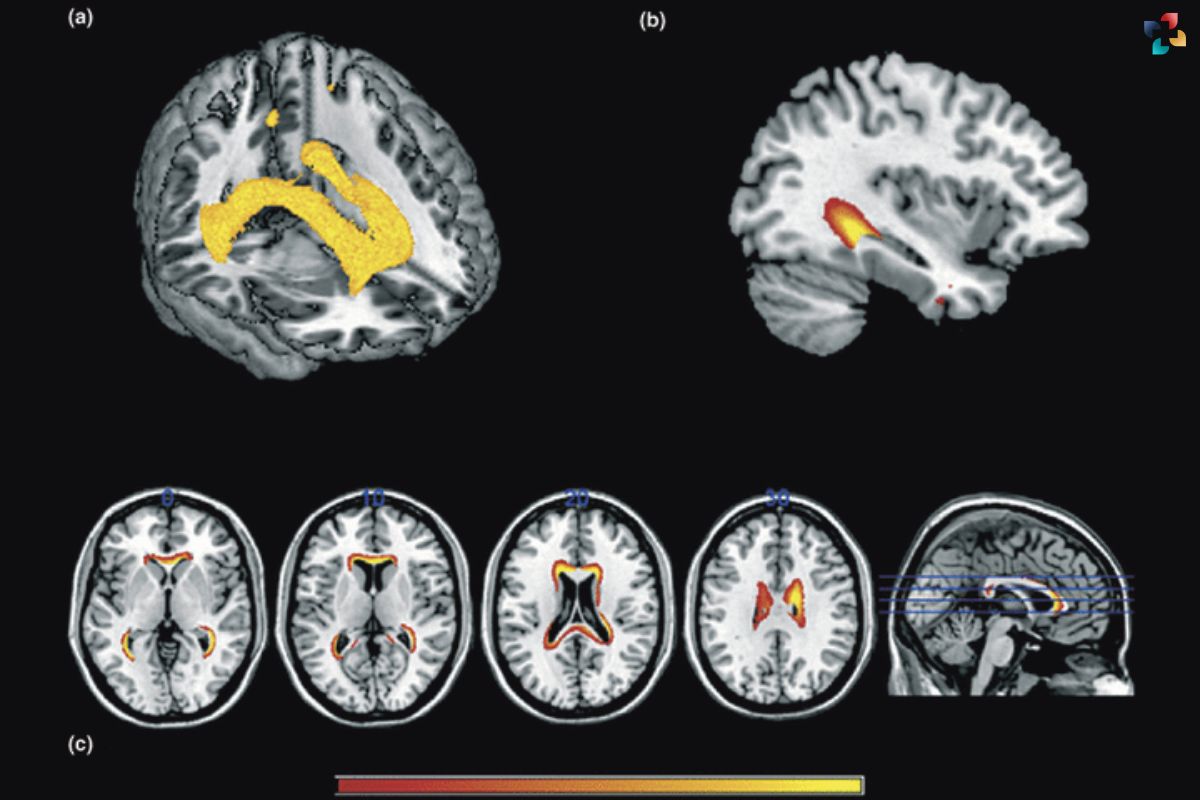
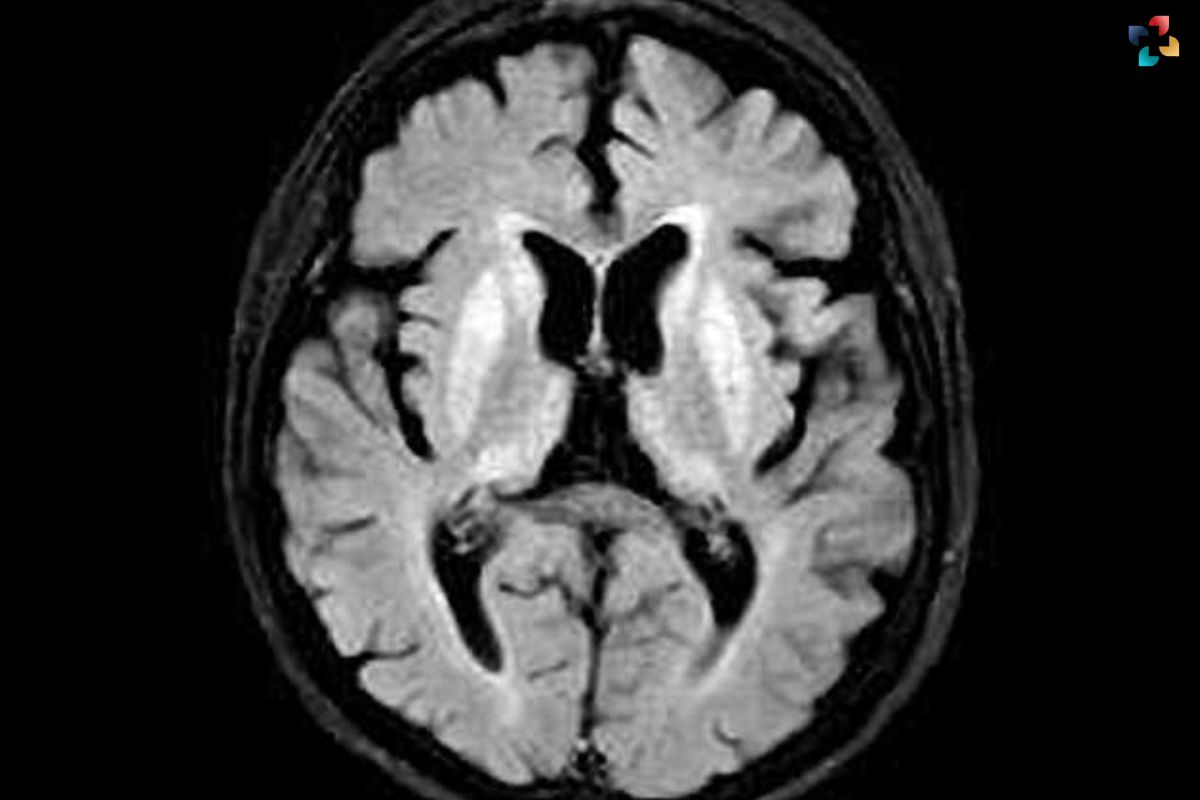
Diagnosing Creutzfeldt-Jakob Disease presents significant challenges due to its rarity and nonspecific clinical presentation. Clinical evaluation, combined with neuroimaging studies such as MRI and EEG, can aid in the differential diagnosis of CJD from other neurological conditions. Additionally, cerebrospinal fluid analysis and brain biopsy may be performed to detect abnormal prion proteins and confirm the diagnosis of CJD definitively.
In conclusion, Creutzfeldt-Jakob Disease is a rare and devastating neurodegenerative disorder with multiple etiological factors and a rapidly progressive clinical course. Understanding the causes and risk factors associated with CJD is essential for early recognition and timely intervention. Continued research efforts aimed at unraveling the pathophysiology of CJD and developing effective diagnostic and therapeutic strategies are crucial for improving outcomes for affected individuals and their families.
Challenges in Diagnosis

Currently, there is no cure for Creutzfeldt-Jakob Disease, and treatment options are limited to alleviating symptoms and providing supportive care. Management strategies focus on controlling pain, managing behavioral symptoms, and ensuring patient comfort and dignity throughout the course of the disease. Palliative care teams play a crucial role in addressing the physical, emotional, and spiritual needs of both patients and their families, offering guidance and support during this challenging journey.
Research efforts are underway to better understand the underlying mechanisms of Creutzfeldt-Jakob Disease and develop potential therapies to halt or slow its progression. Experimental treatments, including immunotherapies and antiprion drugs, hold promise in targeting abnormal prion proteins and preventing their accumulation in the brain. However, further clinical trials are needed to assess their safety and efficacy in treating CJD.
Conclusion
In conclusion, Creutzfeldt-Jakob Disease remains a rare yet devastating neurodegenerative disorder with no cure currently available. Early recognition of symptoms, accurate diagnosis, and comprehensive supportive care are essential in managing the disease and improving the quality of life for affected individuals and their families. Continued research efforts aimed at unraveling the mysteries of CJD offer hope for future breakthroughs in treatment and ultimately finding a cure for this debilitating condition.
FAQs
1. What are the main symptoms of Creutzfeldt-Jakob Disease?
The primary symptoms of CJD include cognitive impairment (memory loss, confusion), personality changes, behavioral abnormalities, involuntary movements, muscle stiffness, difficulty walking, and profound dementia.
2. How is Creutzfeldt-Jakob Disease diagnosed?
Diagnosis of CJD involves clinical evaluation, neuroimaging studies (MRI, EEG), cerebrospinal fluid analysis, and occasionally brain biopsy to detect abnormal prion proteins, confirming the presence of the disease.
3. Is Creutzfeldt-Jakob Disease hereditary?
While most cases of CJD are sporadic, some are familial and linked to mutations in the PRNP gene. However, familial CJD is relatively rare compared to the sporadic form.
4. Can Creutzfeldt-Jakob Disease be transmitted to others?
Iatrogenic CJD can occur through medical procedures involving contaminated tissues or instruments. Variant CJD, associated with consumption of contaminated beef products, is a concern, although strict food safety measures have reduced its incidence.
5. Is there a cure for Creutzfeldt-Jakob Disease?
Currently, there is no cure for CJD, and treatment focuses on managing symptoms and providing supportive care to improve quality of life. Research into potential therapies, such as immunotherapies and antiprion drugs, is ongoing, but no definitive treatment exists yet.