Imagine waking up to find a mysterious rash spreading across your arm, intensely itchy and red. You’re unsure if it’s a sign of an allergic reaction, an infection, or something more serious. In moments like these, understanding what your skin is communicating becomes crucial.
“The skin provides a barrier to protect the body from invasion by bacteria and other possible environmental hazards that can be dangerous for human health,” said NIH dermatologist Dr. Heidi Kong.
But what happens when skin is attacked? The types of skin rashes we will see in the blog are attacks on the skin and a signal of the internal struggles.
According to the National Cancer Institute, a skin rash is an area of the skin that shows changes in texture or color, appearing inflamed or irritated. It may be red, warm, scaly, bumpy, dry, itchy, swollen, painful, cracked, or blistered. Rashes can be localized or widespread and often indicate an underlying condition like allergies, infections, or skin disorders.
So, how do you recognize them? How do you know what caused these rashes? That’s exactly what we will answer in this blog. We will take a look at all types of skin rashes and how they affect us, and what they mean for our health.
So, without wasting too much time, let’s get straight into it!
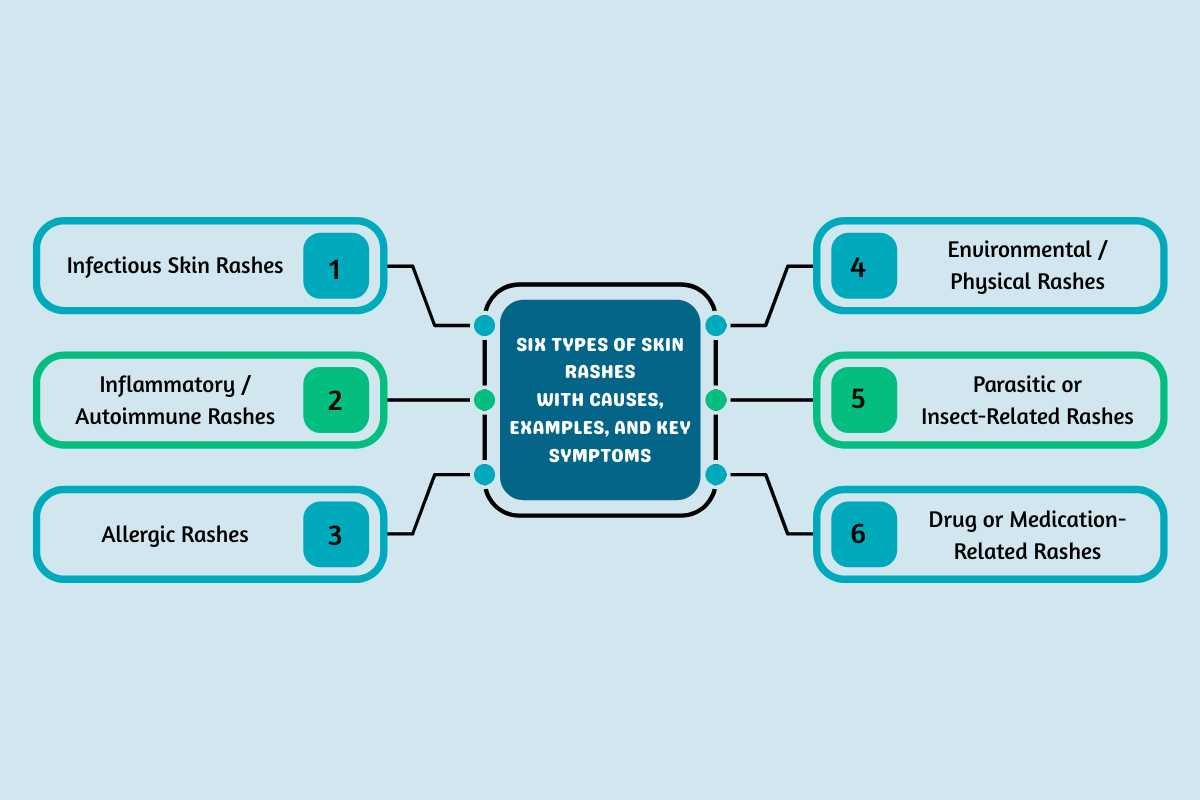
Six Types of Skin Rashes with Causes, Examples, and Key Symptoms
Skin rashes can be categorized into six types. These types are based on the cause of these skin rashes. Knowing them helps us to understand how to treat and prevent them.
Here are the types of skin rashes, their causes, and symptoms:
| Type of Rash | Examples | Causes | Common Symptoms |
|---|---|---|---|
| Infectious Rashes | – Chickenpox- Measles- Shingles- Impetigo- Ringworm- Hand, Foot & Mouth Disease- Scarlet Fever | Infections:- Bacterial- Viral- Fungal | – Redness- Blisters or pustules- Itchiness- Fever or malaise- Lesions that may ooze or crust |
| Inflammatory / Autoimmune Rashes | – Eczema (Atopic Dermatitis)- Psoriasis- Seborrheic Eczema- Lupus Rash- Lichen Planus- Granuloma Annulare | Autoimmune activity- Genetic predisposition- Environmental triggers | – Redness, scaling, swelling- Itchy or painful patches- Patterned rashes (e.g., butterfly rash in lupus) |
| Allergic Rashes | – Contact Dermatitis- Allergy Rashes (Urticaria/Hives) | Allergens (plants, latex, cosmetics)- Irritants (soaps, chemicals, detergents) | – Red, swollen, sometimes blistered skin- Itching or burning at contact site- Possible welts |
| Environmental / Physical Rashes | – Heat Rash (Miliaria/Prickly Heat)- Diaper Rash | Heat and sweat retention- Friction and moisture- Tight or occlusive clothing/diapers | – Small red bumps- Itching, irritation- Blistering in severe cases |
| Parasitic or Insect-Related Rashes | – Scabies- Flea Bites- Bug Bites | Parasite infestations (mites, fleas)- Insect bites | – Intense itching- Red bumps or blisters- Clusters or linear tracks on skin |
| Drug or Medication-Related Rashes | – Drug eruptions (varied presentation) | Allergic or sensitivity reaction to medications | – Sudden widespread redness- Itchiness or hives- Possible blistering |
Let’s talk about each of the types of skin rashes given above. In the next couple of minutes, we will try to understand their causes, remedies, and most importantly, when to visit a dermatologist.
1. Infectious Skin Rashes
This type of skin rash is caused by microorganisms invading your immune system. An attack by viruses, bacteria, fungi, etc, can lead to infectious skin rashes. According to a study, infectious skin rashes are the most common types of skin rashes affecting young children. This is due to thinner, more delicate skin and developing immune systems.
Examples of Infectious Skin Rashes:
- Viral rashes: Measles, Rubella, Chickenpox (Varicella), Shingles (Herpes Zoster), Fifth Disease (Parvovirus B19), Roseola, Mononucleosis (Epstein-Barr Virus), Hand, Foot, and Mouth Disease, Zika Virus, West Nile Virus.
- Bacterial rashes: Impetigo, Scarlet Fever, Cellulitis, Lyme disease, Kawasaki Disease, Folliculitis.
- Fungal rashes: Ringworm (Tinea), Candidiasis.
- Parasitic rashes: Scabies, lice, other mite infestations.
Causes: The causes are varied for each subtype. Viral transmission occurs via respiratory droplets, direct contact, or contaminated surfaces. Bacterial rashes are spread by direct skin contact, contaminated surfaces, or respiratory droplets (e.g., impetigo and cellulitis). And fungal and parasitic rashes spread by contact with contaminated surfaces, animals, or people (e.g., mites causing scabies, or fungi causing ringworm).
Symptoms: The general rash can appear as red or discolored patches, bumps, blisters, oozing sores, crusting, or swelling. Systemic signs often go along with these rashes, including fever, chills, tiredness, headache, joint pain, or respiratory symptoms.
Measles starts on the face and spreads to the trunk with high fever and cough. Chickenpox shows multiple stages of rash, itchy blisters, and fever. Impetigo is a crusty yellow sore.
Fifth Disease is known for the “slapped cheek” red rash. Ringworm shows circular, scaly, itchy patches. Scabies causes intense itching, especially at night, with visible burrows.
Note: Coloration may depend on skin tone, appearing pink/red on lighter skin, but purplish/gray on darker skin.
2. Inflammatory / Autoimmune Rashes
When your immune system attacks your skin, it can lead to some devastating results. Inflammatory and autoimmune rashes result from the body’s immune system mistakenly attacking its own skin cells. This can cause inflammation and varied skin changes. These conditions often include chronic or relapsing symptoms. They may affect other organs beyond the skin. And therefore, it is advised to visit a skin specialist in such cases.
Examples of Autoimmune Rashes:
- Psoriasis: Chronic plaque formation, red, thick, scaly patches often on elbows, knees, scalp, and lower back. It’s the most prevalent autoimmune skin condition, prone to itching and discomfort.
- Lupus (Systemic and Cutaneous): Lupus can cause facial “butterfly” rashes, discoid patches, or sun-induced lesions. Systemic lupus also affects organs like the kidneys, joints, and the heart.
- Scleroderma: Characterized by hard, shiny, thickened skin patches, which may also affect connective tissues in organs.
- Dermatomyositis: Muscle weakness with distinctive reddish or purple rashes on the face (heliotrope rash), hands, and other sun-exposed areas.
- Eczema (Atopic Dermatitis): A Chronic itchy rash, often associated with asthma or hay fever, may be triggered by immune dysfunction.
- Vitiligo: White patches from autoimmune destruction of pigment cells.
- Bullous Pemphigoid: Firm, itchy blisters, mostly in those over 70.
- Vasculitis: Purple spots, rashes, ulcers from autoimmune inflammation of blood vessels.
Causes: The root of these types of skin rashes is an Autoimmune Reaction, where the immune system misidentifies healthy skin as foreign. This leads to persistent inflammation, redness, or blistering.
A genetic factor is often involved, as many autoimmune skin disorders are seen more often in families. Triggers like physical trauma, sun exposure, stress, or certain medications can provoke flares or the initial onset in susceptible individuals.
Symptoms: Symptoms include inflamed, red, or discolored skin (ranging from pink, purple, brown, or white), and are often accompanied by itching or pain. One may observe scaly, thick, or raised patches (as in psoriasis) or blistering or ulceration (in bullous pemphigoid).
A key feature in conditions like lupus is sensitivity to sunlight, where rashes may appear or worsen with sun exposure. Additionally, Dermatomyositis may involve muscle pain or weakness.
3. Allergic Rashes
Allergic rashes are skin reactions caused by the immune system’s abnormal response to an allergen or irritant. This reaction often results in redness, swelling, itching, bumps, or blisters.
These rashes are distinct from those caused by infection or autoimmunity, as they arise only in response to external or internal allergens. It is suggested to visit an allergist to find out the allergens and prevent these types of skin rashes.
Examples of Allergic Rashes:
- Contact Dermatitis (Allergic/Irritant): Appears where the allergen touched; often red, itchy, may blister or ooze. Common causes: latex, cosmetics, soaps, poison ivy.
- Hives (Urticaria): Raised, red, itchy welts that can appear anywhere and move around the body. Triggered by foods, medications, infections, or unknown causes. Hives usually resolve within hours to days, but can recur.
- Allergic Eczema (Atopic Dermatitis): A Chronic condition marked by recurring itchy, scaly, dry patches, often linked to other allergies or asthma.
- Photoallergic Dermatitis: Rash triggered by sun exposure in combination with allergens like some sunscreens or cosmetics.
Causes: Causes are related to exposure and fall into three main categories. First, direct contact with allergens or irritants is a cause. These include things like poison ivy, latex, soaps, detergents, cosmetics, and metals like nickel.
Second, consumption of allergenic foods (like shellfish) or medications can cause widespread rashes. Third, environmental triggers such as pollen, dust mites, or animal dander can cause skin reactions in sensitive people. Finally, insect stings or bites can also lead to local or body-wide allergic responses.
Symptoms: Symptoms typically include an itching, burning, or stinging sensation, accompanied by redness or swelling of the skin, and the appearance of raised welts, bumps, or blisters.
With repeated exposure, the skin may exhibit oozing, crusting, or scaling. In severe reactions, swelling of the face, lips, or airways (anaphylaxis) may occur and necessitate urgent care.
Also Read:
- Why Skin Rashes Keep Coming Back and What You Can Do?
- Demystifying Red Spots on Skin: Causes, Symptoms, and Treatment Options
4. Environmental / Physical Rashes
These types of rashes are skin reactions triggered by environmental factors. These factors include temperature extremes, sun exposure, humidity, friction, and contact with certain plants or chemicals—not by infection, allergy, or autoimmunity.
These rashes can affect anyone but may be more common in people exposed to certain environmental conditions for extended periods.
Examples of Environmental Rashes:
- Heat Rash (Prickly Heat): Small, itchy, red or pink bumps caused by sweat gland blockage in hot, humid climates.
- Sunburn: Painful, red skin with possible blistering after UV exposure; may peel as it heals.
- Contact Dermatitis (Irritant): Red, swollen, sometimes blistering rash from friction or exposure to non-allergenic irritants like detergents, soaps, or solvents.
- Friction Rash: Raw, irritated skin where repeated rubbing occurs.
- Cold-Induced Rash: Chilblains or frostbite after exposure to cold.
- Plant-Induced Rash: Localized welts or hives following plant contact (e.g., stinging nettle, poison ivy).
- Pollution-Related Rashes: Increased eczema, atopic dermatitis, pigmentation (melasma) in polluted regions.
Causes: Heat and humidity block sweat glands, causing Heat Rash (miliaria). Cold exposure can lead to rashes, frostbite, or chilblains, typically on the extremities. Sunlight and UV radiation cause sunburn or conditions like polymorphic light eruption.
Environmental pollutants increase the risk of eczema and melasma. Friction and pressure from clothes or movement cause irritant rashes. Lastly, water and chemicals (like detergents) cause irritant contact dermatitis, and contact with plants like stinging nettle causes localized rashes.
Symptoms: Symptoms involve redness, itching, stinging, or burning in affected areas, along with small bumps or blisters. One may also see scaling, dryness, or swelling. Sensitivity or pain is common with sunburn and frostbite. The defining feature is that the rash appears only after physical exposure to a trigger like heat, cold, sun, friction, or chemicals.
5. Parasitic or Insect-Related Rashes
Parasitic and insect-related skin rashes are caused by infestations or bites from organisms such as mites, lice, fleas, and worms. These rashes may be intensely itchy and show distinctive patterns depending on the organism involved.
These skin rashes are generally highly pruritic. They may be accompanied by additional symptoms such as swelling, pain, or visible bug bites. They tend to require both symptomatic relief and targeted antiparasitic treatment for complete resolution.
Examples of Parasitic Skin Rashes:
- Scabies: Caused by the burrowing mite Sarcoptes scabiei, resulting in intensely itchy, pimple-like linear rash, sores, and crusty patches, especially in finger webs, wrists, and elbows.
- Pediculosis (Lice): Includes head lice, body lice, and pubic lice, leading to an itchy scalp or skin, visible insects or nits, and sometimes secondary infection from scratching.
- Bedbug infestation: Itchy, red bumps or welts, often clustered and appearing after sleep, may cause allergic reactions.
- Flea bites (Pulicosis): Small, itchy papules or welts, may cause acute infant pruritus in sensitized children; flea bites often appear in clusters around the ankles and legs.
- Tungiasis: Caused by the sand flea Tunga penetrans, which burrows into the skin (especially feet/toes), causing a painful yellowish nodule with a black spot in the center, surrounded by intense pruritus and sometimes secondary infection.
- Cutaneous Larva Migrans: Serpiginous, linear, and intensely itchy rash resulting from burrowing nematode larvae, usually after contact with contaminated sand or soil (from dog/cat feces).
- Swimmer’s Itch (Cercarial Dermatitis): Allergic rash after contact with water containing specific parasite larvae from infected snails; causes tingling, burning, small pimples, and blisters.
- Myiasis: Skin boil-like lesions caused by the larvae of some fly species.
- Tick bites (Lyme Disease): Bullseye-pattern rash (erythema migrans) a few days after a bite, sometimes accompanied by systemic symptoms.
Causes: These rashes stem from direct infestation or feeding. Scabies is caused by the Sarcoptes scabiei mite burrowing into the skin. Lice (Pediculosis) feed on blood. Flea bites inject saliva, causing irritation. Bedbugs feed while injecting saliva with anticoagulants.
Tungiasis results from the sand flea penetrating the skin. Cutaneous Larva Migrans happens when hookworm larvae penetrate from contaminated sand. Other causes are the allergic reaction to parasite larvae known as Swimmer’s itch, and Tick bites, which can transmit infections like Lyme disease.
Symptoms: Symptoms include intense itching (pruritus), often worse at night or with heat. One can observe red, raised bumps or papules at bite or burrow sites, and sometimes linear or serpiginous tracks or tunnels on the skin (Scabies or Larva Migrans).
Blisters, crusting, or excoriations from scratching are common, as is local swelling. In some cases, painful nodules (tungiasis) or hive-like reactions occur, and there is a risk of secondary bacterial infections due to scratching.
6. Drug or Medication-Related Rashes
Now these are types of skin rashes that are a reaction to medications. They occur when the body’s immune system reacts adversely to a medication, or the medication itself causes direct skin toxicity. These rashes can range from mild and common to severe and potentially life-threatening. And it is advised to visit a doctor before they become life-threatening.
Examples of Drug-related Rashes:

- Exanthematous (Maculopapular): Widespread red flat and raised patches, often from antibiotics or anti-seizure drugs.
- Urticaria (Hives) / Angioedema: Raised itchy welts or swelling, commonly caused by NSAIDs, penicillin, or ACE inhibitors.
- Fixed Drug Eruption: Round dark-red or violet patches that may blister, linked to NSAIDs or antibiotics.
- Drug-Induced Vasculitis: Tiny purple or brown blistering spots, often due to penicillin or allopurinol.
- Stevens-Johnson Syndrome / TEN: Painful dark-red patches with skin peeling and mucosal damage, triggered by antibiotics or anti-seizure meds.
- DRESS Syndrome: Widespread rash with fever and organ involvement, usually from allopurinol or carbamazepine.
- Photosensitivity: Sunburn-like rash triggered by sunlight, caused by tetracyclines, NSAIDs, or sulfa drugs.
Causes: The main cause of these rashes is an immune-driven allergic reaction. This happens when your immune system becomes sensitive to a medication and reacts strongly when you take that drug again. Other medications cause drug reactions that are non-allergic; these simply lead to skin changes, like acne-like rashes or light sensitivity, without involving a true immune allergy.
In cases of photosensitivity, certain drugs make your skin extra sensitive to sunlight, which results in sunburn-like rashes after exposure to UV light. The most worrisome reactions are called Severe Cutaneous Adverse Reactions (SCARs). These are rare but very serious and potentially deadly conditions, including Stevens-Johnson syndrome (SJS), Toxic Epidermal Necrolysis (TEN), and DRESS.
Symptoms: Symptoms include a red or purple rash, often symmetrical and widespread, with raised bumps, hives, or blistering in some types. Itching or tenderness is common. In severe cases, blistering, peeling, mucous membrane sores, fever, and systemic symptoms like organ involvement may occur. The rash onset can be rapid (hours) or delayed (days to weeks) after drug exposure.
Also Read:
- Rashes in Groin Area: Causes, Symptoms, and How to Treat Them?
- How to Treat Bacterial Skin Infections: An Essential Guide
How Can You Prevent Different Types of Skin Rashes Effectively?

- Protective Clothing and Sunscreen: Wear protective clothing and broad-spectrum sunscreen to shield skin from sunburn, UV damage, and environmental irritants like pollution and insect bites.
- Identify and Avoid Triggers: Know your allergens or irritants (e.g., certain plants, chemicals, soaps, metals, foods) and avoid contact. Patch testing may help identify allergens for allergic rashes.
- Gentle Skin Care: Use mild, fragrance-free, hypoallergenic soaps and moisturizers to maintain the skin barrier and reduce irritation risk. Avoid harsh chemicals and exfoliants that dry or damage skin.
- Good Hygiene: Regularly clean skin with warm (not hot) water and mild cleansers to remove dirt, sweat, and microbes that contribute to infections or irritation.
- Avoid Sharing Personal Items: Prevent transmission of infectious or parasitic rashes by not sharing towels, bedding, or clothing, especially in communal or athletic settings.
- Manage Heat and Moisture: Wear breathable, loose clothing and keep skin dry to prevent heat rashes or fungal infections. Use air conditioning or fans in hot environments.
- Hydrate and Nourish Skin: Drink sufficient water and use emollient moisturizers to keep skin hydrated and support barrier function, which helps prevent eczema flare-ups and irritant contact dermatitis.
- Prompt Medical Attention: Seek early diagnosis and treatment for rashes to prevent worsening or complications, especially for drug reactions and severe infectious rashes.
Here is a table for specific prevention tips according to the types of skin rashes:
| Rash Type | Prevention Tips |
|---|---|
| Infectious Rashes | Vaccination (e.g., chickenpox), avoiding contact with infected individuals, and maintaining good hygiene. |
| Inflammatory Rashes | Avoid known triggers such as allergens, stress, or sun exposure; maintain a regular moisturizing skincare routine. |
| Allergic Rashes | Identify and avoid allergens. Use hypoallergenic skincare products, and undergo patch testing if needed. |
| Environmental Rashes | Use antioxidant skincare and sunscreen, avoid pollutants, and keep the skin well-hydrated. |
| Parasitic / Insect Rashes | Use insect repellents, maintain clean living conditions, and avoid contaminated soil or water sources. |
| Drug-Related Rashes | Inform healthcare providers of drug allergies, avoid implicated medications, and consider genetic screening when relevant. |
When Should You See a Dermatologist for a Skin Rash?
According to WebMD, you should consider visiting a skin specialist or dermatologist if you experience any of the following in relation to a skin rash:
- The rash appears suddenly and spreads quickly over your entire body.
- There are signs of infection, such as pus, thick liquid, or sores that won’t heal.
- The rash is painful, oozing, crusty, or shows red streaks, indicating potential infection.
- You have a fever of 100°F or higher along with the rash, which could indicate a systemic infection or illness.
- The rash is located near your eyes, mouth, or genitals, or in warm folds of the skin, like between fingers or under breasts.
- The rash is causing significant discomfort, such as intense itching or burning, or if home remedies aren’t effective within a couple of weeks.
- The rash is associated with other symptoms like joint pain, muscle aches, or difficulty swallowing, which could suggest a more serious underlying condition.
WebMD emphasizes that prompt medical attention is essential if the rash is linked with signs of infection, systemic symptoms, or if it covers a large area and worsens despite initial care.
According to the AAD (American Academy of Dermatology), here are some signs that your skin rash is a serious problem:
- A rash over most of your body.
- A rash that blisters or turns into open sores or raw skin.
- Fever or illness with a rash.
- A rash that spreads rapidly.
- A painful rash.
- A rash involving the eyes, lips, mouth, or genital skin.
What Tests Help Diagnose the Exact Type of Skin Rash?
There are some diagnostic tests that help us determine the type of rash and its causes. Here’s what they are:
- Patch Testing: Used primarily for allergic contact dermatitis, small patches containing common allergens are applied to the skin and observed over 48-96 hours for reactions.
- Skin Biopsy: A tiny skin sample is taken under local anesthesia for microscopic examination. This helps confirm diagnosis in unclear or persistent cases and differentiate between infectious, autoimmune, or neoplastic causes.
- Blood Tests: May include complete blood count, inflammatory markers, allergy testing, or specific serologies to detect infections or systemic involvement.
- Other Tests: Skin scrapings, microscopy, and cultures for fungi or bacteria, prick testing for immediate allergic reactions, and dermoscopy (magnified skin examination) are used as needed based on clinical suspicion.
Conclusion
Skin serves as the body’s communication system. It gives us signs of internal issues, from minor irritations to serious diseases. Knowing the distinct traits of different types of skin rashes allows you to identify the trigger. Promptly reading this language is crucial for effective care.
Never ignore persistent or severe symptoms. Learning about the types of skin rashes empowers you to seek a timely medical diagnosis. They make sure you receive the correct treatment and protection for your skin, on time.
FAQs
1. Are hormonal rashes always caused by pregnancy or menopause?
No, hormonal rashes can also signal thyroid issues, PCOS, or result from monthly menstrual cycle fluctuations, particularly around puberty.
2. Can stress cause a rash, or is it always infectious or allergic?
Stress doesn’t directly cause a rash, but it can trigger flare-ups of existing conditions like eczema, psoriasis, or hives by weakening the immune response.
3. How do I know if I need a prescription versus an over-the-counter cream?
If a rash is painful, blistering, accompanied by fever, spreading rapidly, or doesn’t improve with OTC treatment after a few days, see a doctor.







