Introduction:
Living with stomach ulcers can be uncomfortable and disruptive to daily life. However, managing your condition through a well-balanced diet can significantly alleviate symptoms and promote healing. In this comprehensive guide, we’ll explore the ins and outs of a stomach ulcer diet, including foods to eat and avoid, meal planning tips, and lifestyle adjustments to support digestive health.
Understanding Stomach Ulcers:
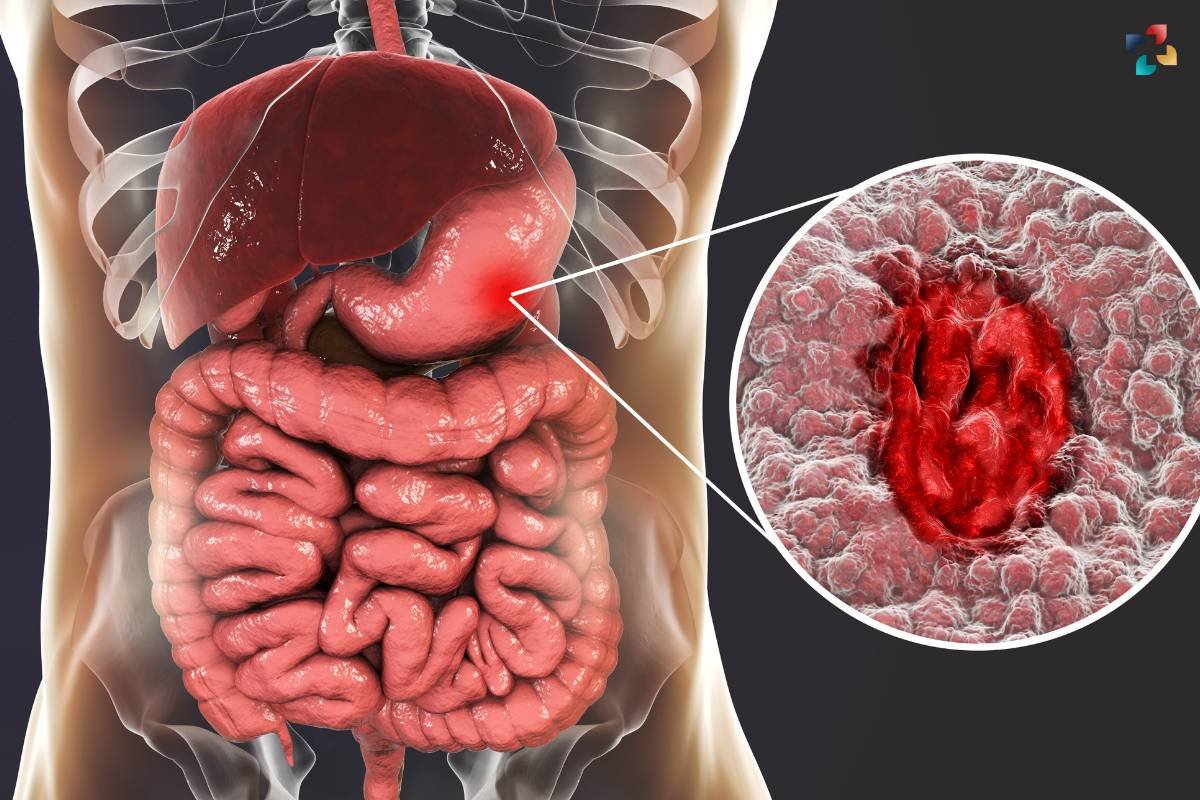
Before delving into dietary recommendations, let’s briefly discuss what stomach ulcers are and how they develop. Stomach ulcers, also known as gastric ulcers, are open sores that form on the lining of the stomach. These ulcers can be caused by various factors, including infection with Helicobacter pylori bacteria, prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs), excessive alcohol consumption, and smoking.
Symptoms of stomach ulcers may include abdominal pain or discomfort, bloating, heartburn, nausea, and vomiting. In severe cases, ulcers can lead to complications such as internal bleeding or perforation of the stomach lining. While medical treatment is essential for managing ulcers, adopting a stomach ulcer diet can complement traditional therapies and support overall gut health.
The Role of Diet in Managing Stomach Ulcers:

A well-planned diet plays a crucial role in managing stomach ulcers by reducing irritation to the stomach lining, promoting healing, and preventing flare-ups. The primary goals of a stomach ulcer diet are to:
- Minimize gastric acid production: Certain foods can trigger excess stomach acid production, exacerbating ulcer symptoms. Avoiding these triggers and consuming foods that help neutralize acid can alleviate discomfort.
- Protect the stomach lining: Some foods have soothing properties that can coat and protect the stomach lining, reducing irritation and inflammation.
- Support digestive health: A balanced diet rich in nutrients, fiber, and probiotics can promote overall digestive health and enhance the body’s ability to heal ulcers.
- Foods to Include in a Stomach Ulcer Diet: When planning meals for stomach ulcer relief, focus on incorporating the following stomach-friendly foods:
- High-fiber fruits and vegetables: Opt for fruits like apples, bananas, and berries, as well as vegetables such as spinach, kale, and broccoli. These foods are rich in fiber, which aids digestion and helps prevent constipation.
- Lean proteins: Choose lean sources of protein such as skinless poultry, fish, tofu, and legumes. Protein is essential for tissue repair and supports overall health.
- Whole grains: Include whole grains like brown rice, quinoa, oats, and whole wheat bread in your diet. These grains provide essential nutrients and fiber without aggravating ulcer symptoms.
- Healthy fats: Incorporate sources of healthy fats, such as olive oil, avocados, nuts, and seeds, into your meals. These fats support cardiovascular health and may help reduce inflammation in the body.
- Fermented foods: Probiotic-rich foods like yogurt, kefir, sauerkraut, and kimchi contain beneficial bacteria that promote gut health and may help reduce the risk of H. pylori infection.
Foods to Avoid in a Stomach Ulcer Diet:

To prevent irritation and exacerbation of ulcer symptoms, it’s important to limit or avoid the following foods:
- Spicy foods: Spicy dishes, hot peppers, and chili peppers can increase stomach acid production and aggravate ulcer pain.
- Acidic foods and beverages: Citrus fruits, tomatoes, vinegar, and citrus juices are acidic and can irritate the stomach lining. Similarly, carbonated beverages and caffeinated drinks should be consumed in moderation.
- Fried and fatty foods: Greasy, fried foods and high-fat dishes can slow digestion and may contribute to acid reflux and discomfort.
- Alcohol and tobacco: Both alcohol and tobacco can weaken the stomach lining and increase the risk of ulcers. Limit or avoid alcohol consumption, and consider quitting smoking to support ulcer healing.
- NSAIDs and aspirin: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin can irritate the stomach lining and worsen ulcer symptoms. Consult your healthcare provider for alternative pain relief options if necessary.
Meal Planning Tips for Stomach Ulcer Relief:
Creating a stomach ulcer diet plan requires careful consideration of individual preferences, dietary restrictions, and ulcer triggers. Here are some meal-planning tips to help you navigate your dietary needs:
- Eat smaller, more frequent meals: Consuming smaller meals throughout the day can help prevent excess stomach acid production and reduce the likelihood of discomfort.
- Chew food thoroughly: Chew food slowly and thoroughly to aid digestion and minimize the workload on your stomach.
- Stay hydrated: Drink plenty of water throughout the day to maintain hydration and support digestive function. Limit intake of caffeinated and carbonated beverages, as they can exacerbate ulcer symptoms.
- Keep a food diary: Keeping track of your dietary intake and any associated symptoms can help identify trigger foods and patterns that worsen ulcer symptoms.
- Consult a registered dietitian: If you’re unsure how to create a stomach ulcer diet plan or need personalized guidance, consider consulting a registered dietitian with experience in digestive health.
Lifestyle Adjustments to Support Digestive Health:
In addition to dietary modifications, certain lifestyle changes can further support digestive health and ulcer management:
- Manage stress: Chronic stress can exacerbate ulcer symptoms and increase gastric acid production. Practice stress-reduction techniques such as meditation, yoga, deep breathing exercises, or spending time outdoors to promote relaxation.
- Get regular exercise: Engaging in regular physical activity can improve digestion, reduce inflammation, and support overall well-being. Aim for at least 30 minutes of moderate exercise most days of the week.
- Prioritize sleep: Adequate sleep is essential for digestive health and overall healing. Aim for 7-9 hours of quality sleep each night to support ulcer recovery and reduce stress levels.
- Avoid eating before bedtime: To prevent acid reflux and discomfort, avoid eating large meals or heavy snacks close to bedtime. Allow at least 2-3 hours for digestion before lying down.
- Follow your treatment plan: Be sure to adhere to any medical treatment prescribed by your healthcare provider, including medications to reduce stomach acid, antibiotics for H. pylori infection, or other therapies as needed.
Conclusion:
A stomach ulcer diet plays a crucial role in managing symptoms, promoting healing, and supporting overall digestive health. By focusing on nutrient-rich foods, avoiding triggers, and making lifestyle adjustments, individuals with stomach ulcers can effectively manage their condition and improve their quality of life. Consult with a healthcare provider or registered dietitian to create a personalized stomach ulcer diet plan tailored to your specific needs and preferences. With the right approach, you can nourish your gut and embark on the path to optimal digestive wellness.
In conclusion, adopting a stomach ulcer diet can be a powerful tool in managing symptoms, promoting healing, and supporting overall digestive health. By incorporating stomach-friendly foods, avoiding triggers, and making lifestyle adjustments, individuals can effectively manage their condition and improve their quality of life. Remember to consult with a healthcare provider or registered dietitian to create a personalized stomach ulcer diet plan that meets your unique needs and preferences. With the right approach, you can nourish your gut and embark on the path to optimal digestive wellness.
Peptic Ulcer Disease: Understanding Causes, Symptoms, and Treatment Options
Peptic ulcer disease (PUD) is a prevalent gastrointestinal disorder characterized by open sores, known as ulcers, that develop on the lining of the stomach, small intestine, or esophagus.







