Vestibular schwannoma, another name for acoustic neuroma, is a rare type of noncancerous tumor that grows on the vestibular nerve, which links the brain and inner ear. Acoustic neuromas are benign in origin, but because they are located close to important cranial nerves, they can produce serious symptoms and consequences. The complexities of acoustic neuroma, including its clinical symptoms, diagnostic techniques, treatment modalities, and the most recent developments in management tactics, are covered in detail in this extensive reference.
Understanding Acoustic Neuroma:
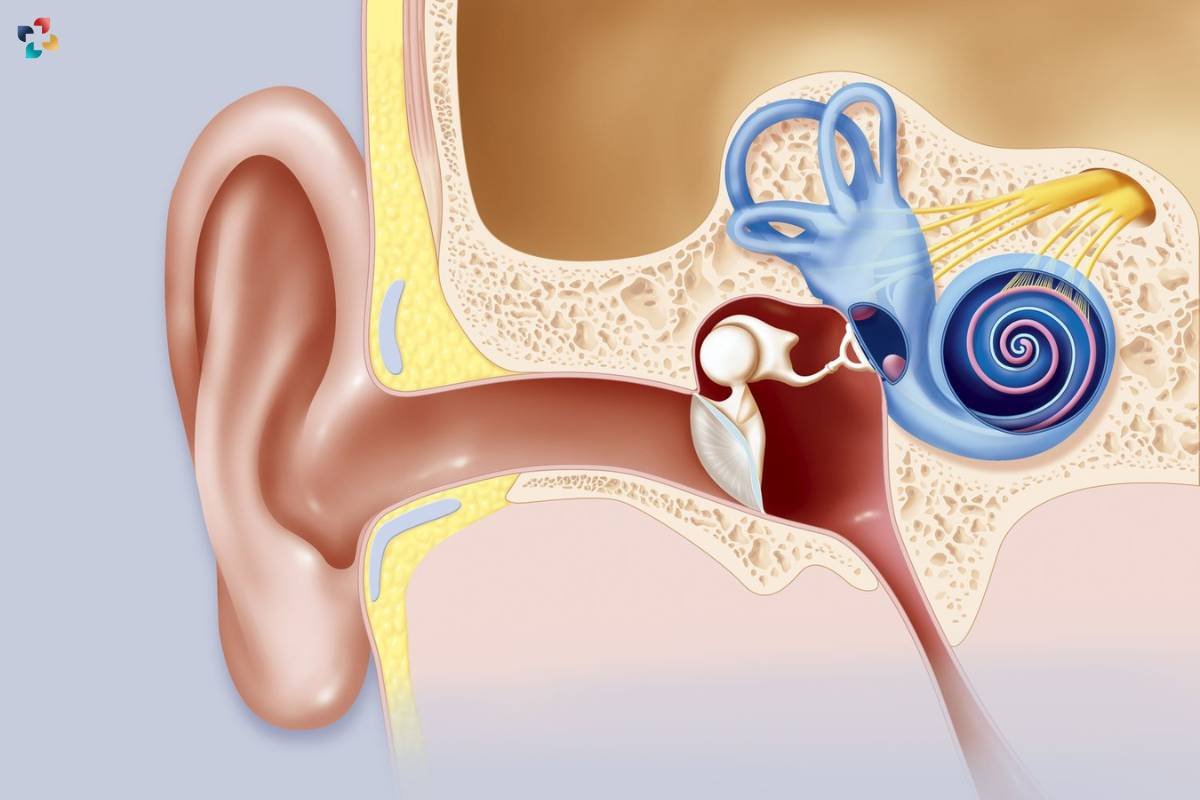
Acoustic neuroma arises from the Schwann cells surrounding the vestibular nerve, typically affecting the vestibular portion known as the superior vestibular nerve. These tumors grow slowly over time, exerting pressure on nearby structures such as the cochlear nerve responsible for hearing and the facial nerve controlling facial movement and sensation. While the exact cause of acoustic neuroma remains unclear, certain risk factors such as neurofibromatosis type 2 (NF2) and exposure to high-dose radiation may increase the likelihood of tumor development.
Clinical Presentation and Symptoms:

The symptoms of acoustic neuroma can significantly impact an individual’s quality of life and functional abilities. Unilateral hearing loss, often the earliest sign, may initially be subtle but progressively worsens over time as the tumor grows and affects the auditory nerve. Tinnitus, described as a persistent ringing or buzzing sensation in the affected ear, can be distressing and intrusive, further exacerbating the auditory impairment.
Vertigo and imbalance, stemming from vestibular nerve involvement, can disrupt mobility and spatial orientation, leading to falls and accidents. Facial numbness or weakness may affect facial expression and sensation, impacting interpersonal interactions and self-esteem. Headaches, though nonspecific, can be debilitating and contribute to overall discomfort and distress. The insidious onset and nonspecific nature of these symptoms underscore the importance of timely evaluation and diagnosis to initiate appropriate management strategies and optimize patient outcomes.
Diagnostic Approaches:
Diagnosing acoustic neuroma typically involves a combination of clinical evaluation and imaging studies. Audiometric testing, including pure tone audiometry and speech audiometry, helps assess hearing loss and discriminate between conductive and sensorineural hearing impairments. Magnetic resonance imaging (MRI) with gadolinium contrast is the imaging modality of choice for visualizing acoustic neuroma, providing detailed anatomical information and delineating tumor characteristics such as size, location, and relationship to surrounding structures.
Treatment Modalities:

In cases of small and asymptomatic acoustic neuromas, observation with regular monitoring through imaging studies may be recommended, particularly for elderly patients or those with significant comorbidities who may not tolerate invasive interventions well. Microsurgical resection, performed by neurosurgeons specialized in skull base surgery, aims to achieve complete tumor removal while preserving facial nerve function and hearing whenever feasible.
Stereotactic radiosurgery, such as Gamma Knife or CyberKnife, delivers highly focused radiation beams to the tumor with minimal damage to surrounding tissues, offering a non-invasive alternative for patients who are poor surgical candidates or prefer to avoid surgery. Fractionated radiotherapy, delivered over multiple sessions, may also be considered for larger tumors or as an adjunct to microsurgical resection to enhance tumor control rates.
The selection of the most appropriate treatment modality requires careful consideration of the tumor characteristics, patient preferences, and potential risks and benefits associated with each approach.
Advancements in Management Strategies:
Advancements in technology and treatment techniques have revolutionized the management of acoustic neuroma, offering improved outcomes and reduced morbidity. Minimally invasive surgical approaches, such as endoscopic endonasal surgery and keyhole retro sigmoid craniotomy, enable precise tumor removal with minimal disruption to surrounding structures. Additionally, advanced radiation delivery systems, including proton therapy and intensity-modulated radiotherapy (IMRT), allow for targeted tumor ablation while sparing adjacent healthy tissues.
Furthermore, innovations in imaging modalities, such as high-resolution MRI and functional MRI (fMRI), facilitate preoperative planning and intraoperative navigation, enhancing surgical precision and safety. Intraoperative monitoring techniques, such as facial nerve monitoring and brainstem auditory evoked potentials (BAEPs), help neurosurgeons assess neural integrity in real-time during surgery, reducing the risk of postoperative complications.
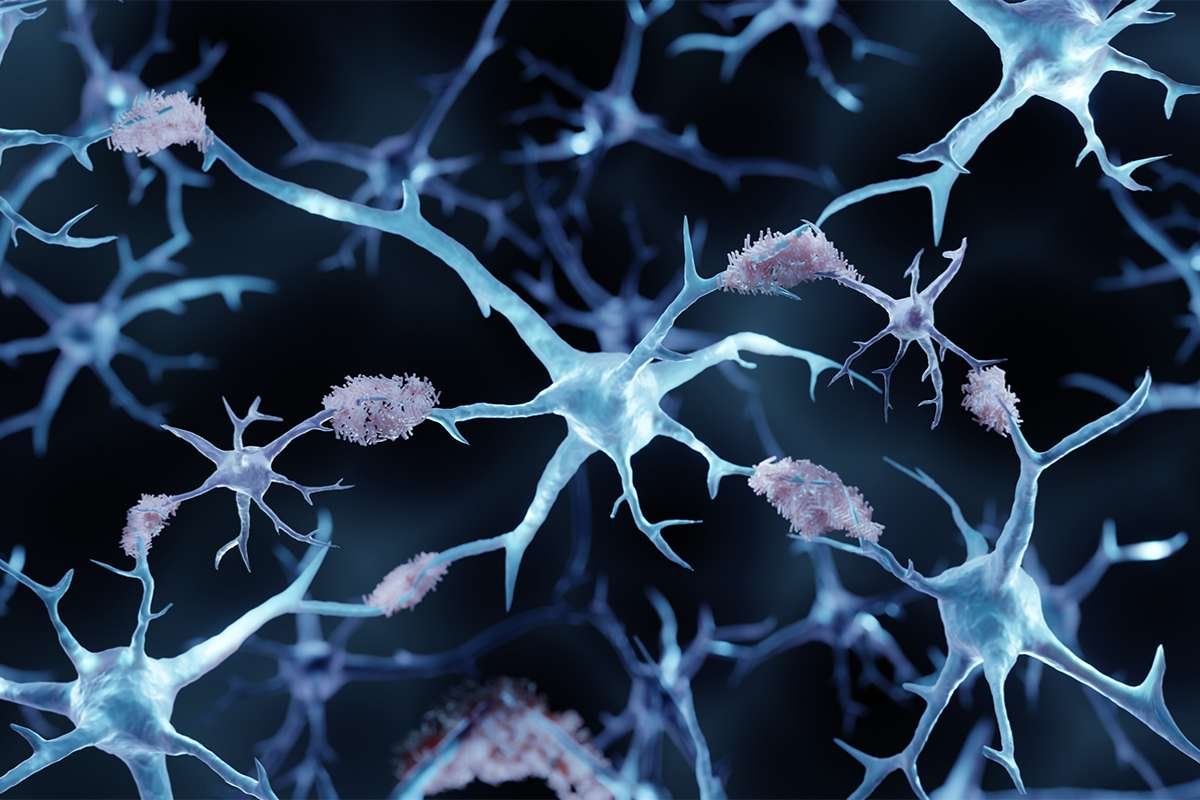
Genetic testing and molecular profiling offer insights into tumor biology and prognostication, guiding personalized treatment strategies and identifying potential therapeutic targets for novel pharmacological interventions. Multidisciplinary tumor boards, comprising neurosurgeons, radiation oncologists, neurologists, and otolaryngologists, foster collaborative decision-making and comprehensive care coordination, ensuring optimal outcomes for patients with acoustic neuroma.
Prognosis and Follow-Up Care:

The prognosis for patients with acoustic neuroma varies depending on factors such as tumor size, growth rate, and treatment modality. While the majority of acoustic neuromas are benign and associated with favorable outcomes, larger tumors or those with intracranial extension may pose greater challenges in management. Long-term follow-up care is essential for monitoring tumor growth, assessing treatment response, and managing potential complications or recurrence. Regular imaging studies and audiometric evaluations are recommended to ensure timely intervention and optimize patient outcomes.
Conclusion:
To sum up, acoustic neuromas offer a complicated clinical picture with a range of symptoms, difficulties with diagnosis, and treatment options. Through an appreciation of the subtleties of the biology of acoustic neuromas and the use of new diagnostic and treatment technologies, medical professionals can offer individualized care that is customized to meet the needs of each patient. To improve patient outcomes and quality of life, it is imperative that interdisciplinary collaboration and ongoing research be done to better understand the pathophysiology of acoustic neuromas and to refine treatment protocols.
FAQs
1. What causes acoustic neuroma?
Acoustic neuroma arises from the Schwann cells covering the vestibular portion of the eighth cranial nerve, also known as the vestibulocochlear nerve. While the exact cause remains unclear, certain factors such as genetic predisposition and exposure to ionizing radiation may increase the risk of developing this tumor.
2. How common is acoustic neuroma?
Acoustic neuroma is relatively rare, accounting for approximately 8-10% of all intracranial tumors. It typically occurs in adults aged 30 to 60 years, with a slight predilection for females.
3. Can acoustic neuroma be cured?
The goal of treatment for acoustic neuroma is to control tumor growth, preserve neurological function, and improve quality of life. While a complete cure may be achievable with surgical resection for small tumors, the management approach depends on factors such as tumor size, location, and patient preferences. In some cases, observation or non-invasive treatments such as radiosurgery may be sufficient to manage the tumor without the need for surgery.
4. What are the potential complications of acoustic neuroma treatment?
Treatment modalities for acoustic neuromas, such as surgery and radiation therapy, carry inherent risks of complications, including hearing loss, facial weakness or paralysis, balance disturbances, cerebrospinal fluid leakage, and injury to adjacent cranial nerves or brain structures. The likelihood and severity of complications depend on various factors, including tumor size, location, and treatment technique.
5. Is genetic testing recommended for individuals with acoustic neuroma?
While most cases of acoustic neuroma occur sporadically without a known genetic predisposition, a small percentage may be associated with hereditary conditions such as neurofibromatosis type 2 (NF2). Genetic testing and counseling may be recommended for individuals with a family history of NF2 or other syndromes linked to acoustic neuroma to assess the risk of developing the tumor and guide surveillance and management strategies.