Diabetes has remained one of the most challenging health problems in the 21st century accounting for a global presence. Despite scientific breakthroughs, better healthcare facilities, and improved literacy rates, the disease continues to burden several sections, especially in middle and low-income countries.
For the diabetes management of type 1 Diabetes, patients require insulin administration 3-4 times a day throughout their lives and their blood sugar level should be regularly monitored to avoid problems like retinopathy(disease of the retina) and risks of cardiovascular diseases(type of disease that affects the heart or blood vessels), for the management of type 2 diabetes, a well-monitored glycemic control is required. Bariatric surgery is increasingly recognized as an effective option for managing type 2 diabetes, which is highly expensive.
So, here are the multiple trends to improve the effectiveness, accessibility, and individualization of diabetes management approaches, with the ultimate goal of optimizing outcomes and enhancing qualities of life for people living with diabetes:
Stem Cell Technology: Novel Therapeutic Approach
Both type 1 and type 2 diabetes result from the 𝛃 cell deficiency of the pancreatic cells, resulting in insufficient insulin secretion. This technology aims either at removing the defects in pancreatic 𝛃 cells or enhancing the sensitivity of the body cells to the action of insulin.
Type 1 and type 2 diabetes results from irregularities in 𝛃 cells function together with insulin resistance in peripheral organs. Mesenchymal stem cell(MSC) therapy has emerged as a promising therapy in the treatment of type 1 diabetes due to its immunosuppressive nature.
MSCs have the potential to differentiate into several mesenchymal cell lineages. The hematopoietic stem cells are the multipotent stem cells that can give rise to all the cell types in blood and also possess immunomodulatory effects. Hence, the transplantation of hematopoietic stem cells has been approved to be a promising therapeutic, resulting in improvement in 𝛃 cell function in newly diagnosed type 1 diabetic patients.
Hence, the application of stem cell technology holds immense prospects in the treatment of diabetes.
Gene Therapy:
The cloning and expression of insulin in the culture cells in the 1970s was a tremendous revolution in the field of medicine. The application of gene therapy in the treatment of diabetes management was suggested as a possible cure.
Gene therapy refers to the insertion of genes into cells to correct genetic abnormalities or enhance cellular function. Gene therapy utilizes viral vectors to deliver genes that boost the growth and survival of 𝛃 cells or to silence genes that contribute to 𝛃 cells destruction. Gene therapy involving the somatic cells of the body includes two methods of gene delivery.
The two methods are:
1. Ex-vivo Gene Therapy
Ex-vivo therapy aims at the generation of cells that possess the properties of 𝛃 cells. This therapy also generates 𝛃 cells for transplantation. It involves genetically modifying cells outside the body to produce therapeutic factors and their subsequent transplantation back into patients.
2. In-vivo Gene Therapy
In-vivo gene therapy, the vector containing the desired gene is directly inserted into the patient. The development of safe and effective vectors remains a challenging task for gene therapists. It is a strategy in which genetic material usually in the form of DNA, is applied to modify the genetic collection of target cells for therapeutic goals.
Statin-Therapy: A New Perspective
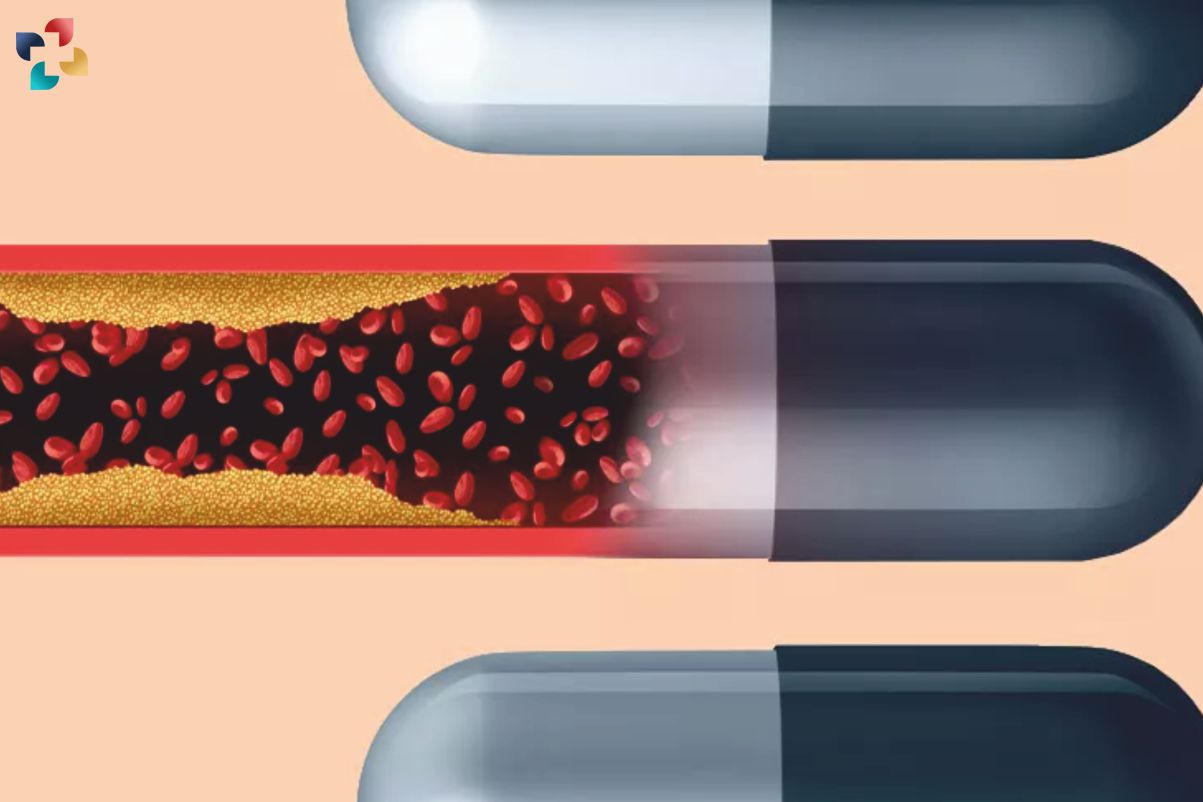
The long-term effects of diabetes include the high risk of cardiovascular diseases, statins are the main line of therapy in reducing cardiovascular risk in patients suffering from type 2 diseases. Statins are defined as inhibitors of 3-hydroxy-3 methylglutaryl coenzyme. They work by blocking a substance that your body needs to make cholesterol.
The enzyme catalyzes the conversion of HMG-CoA to mevalonic acid(It produces terpenes and steroids), the rate of limiting step in the formation of cholesterol. These compounds are highly effective in reducing cholesterol levels as compared to dietary supplements.
Statin therapy reduces low-density protein (LDL) to a significant level thereby greatly decreasing the chances of developing coronary artery disease(It is caused by plaque buildup in the wall of the arteries that supply blood to the heart).
3 statins have a low risk of increasing blood sugar levels:
- Pravastatin
- Fluvastatin
- Pitavastatin
Medical Nutrition Therapy:
American Diabetes Association in 1994 coined the term “Medical Nutrition Therapy” constituting 2 phases, namely, adjudging the nutritional requirement of a person and treatment through counseling and nutrition therapy, respectively.
The objectives of nutritional therapy in diabetes management are to regulate the optimal level of lipids in the blood, ideal body weight, and blood glucose level in the normal range.
This therapy depends on two main factors:
- Patients ‘ based nutritive requirements
- Food preferences
According to recent recommendations, the percentage of carbohydrate intake is based on patients’ intake of protein and fat. A low carbohydrate/high protein diet is popular and may be associated with initial weight loss and improved glycemic control but is difficult to maintain for longer periods.
Protein intake is maintained at 10-20% of all calories; total fat intake should be restricted to less than 30% of total calories; high fiber diet (20-25 grams per day of soluble and insoluble fiber), sodium restriction to 2400-3000 mg/day, alcohol intake (less than 2 drinks per day in men, less than 1 drinks per day in women) and multivitamins should be taken in diet.
Nanotechnology:
The interface of nanotechnology in the treatment of diabetes has introduced novel strategies for glucose measurement and insulin delivery. Research has demonstrated the advantages of glucose sensors and closed-loop insulin delivery approaches in facilitating diabetes management to make it beneficial in both type 1 and type 2 diabetes.
Nanotechnology is based on nanomedical devices. They are microcapsules containing pores which have been a promising tool in the drug delivery approach. These pores are considerably large to allow small molecules to pass oxygen, glucose, and insulins. They are small enough to allow the movement of large immune systems such as immunoglobins and graft-borne(Typically refers to something that is transmitted or carried through grafting, a horticulture technique where tissues from one plant are inserted into those of another so that they will unite and grow as a single plant) virus particles.
Microcapsules containing replacement islets of Langerhans cells, mostly derived from pigs, could be implanted beneath the skin of diabetes patients. This temporarily restores the body’s delicate glucose control feedback loop without the need for powerful immunosuppressants that can leave the patient at serious risk of infection. One of the biggest technological challenges in nanotechnology is the scalability of nano-particles. However recent micro and nanotechnologies have facilitated the insulin administration process through the regulation of insulin delivery constituting pulmonary, nasal, transdermal, and closed-loop delivery.
Conclusion
Recent trends in therapeutic approaches for diabetes management have underscored the importance of personalized care, targeted interventions, and holistic technologies, to effectively address the multifaceted nature of diabetes.
Furthermore, there is growing recognition of the pivotal role of lifestyle modifications, including diet, exercise, and stress management, in glycemic control and improving overall health outcomes for individuals and diabetes.







