Mitochondrial disease encompasses a group of disorders caused by dysfunctional mitochondria, the energy-producing powerhouses of our cells. These diseases can affect multiple organ systems and present a wide array of symptoms, making diagnosis and treatment complex. This article provides a comprehensive overview of mitochondrial disease, exploring its causes, symptoms, diagnostic methods, and treatment options.
What is Mitochondrial Disease?
Mitochondrial disease refers to a group of genetic disorders resulting from mutations in the mitochondrial DNA (mtDNA) or nuclear DNA (nDNA) that affect the function of mitochondria. Mitochondria are responsible for producing adenosine triphosphate (ATP), the energy currency of cells, through a process called oxidative phosphorylation. When mitochondria fail to produce adequate energy, it leads to cellular dysfunction and damage, manifesting as mitochondrial disease.
Causes of Mitochondrial Disease
- Genetic Mutations: The primary cause of mitochondrial disease is genetic mutations. These mutations can be inherited in different ways:
- Maternal Inheritance: Mutations in mtDNA are passed from mother to child, as mitochondria are inherited solely from the egg cell.
- Autosomal Inheritance: Mutations in nDNA can be inherited from either parent and follow autosomal dominant or autosomal recessive patterns.
- De Novo Mutations: These are new mutations that occur spontaneously and are not inherited from parents.
Environmental Factors
While genetic mutations are the main cause, environmental factors can exacerbate mitochondrial dysfunction. Toxins, medications, and infections can negatively impact mitochondrial function, potentially triggering or worsening mitochondrial disease.
Symptoms of Mitochondrial Disease

Mitochondrial disease can affect any organ system, leading to a wide range of symptoms. The severity and combination of symptoms vary greatly among individuals.
Common Symptoms
- Muscle Weakness: Muscle weakness and fatigue are common, as muscles require a lot of energy to function.
- Neurological Issues: Symptoms include seizures, developmental delays, learning disabilities, and movement disorders.
- Cardiovascular Problems: Cardiomyopathy and arrhythmias can occur due to impaired energy production in heart cells.
- Respiratory Issues: Respiratory muscle weakness can lead to breathing difficulties.
- Gastrointestinal Disorders: Symptoms include swallowing difficulties, gastrointestinal dysmotility, and liver dysfunction.
- Hearing and Vision Loss: Sensorineural hearing loss and optic atrophy can result from mitochondrial dysfunction.
Multisystem Involvement
Mitochondrial disease often involves multiple systems, leading to a complex clinical presentation. This multisystem involvement makes diagnosis challenging and necessitates a multidisciplinary approach to management.
Diagnosing Mitochondrial Disease
Diagnosing mitochondrial disease requires a thorough clinical evaluation, detailed family history, and specialized tests. Due to its complexity, a definitive diagnosis often involves multiple steps and the collaboration of various specialists.
Clinical Evaluation
The first step in diagnosing mitochondrial disease is a comprehensive clinical evaluation. This includes:
- Medical History: Detailed family and medical history to identify patterns of symptoms and inheritance.
- Physical Examination: Thorough physical examination to assess signs of muscle weakness, neurological deficits, and other abnormalities.
Laboratory Tests
Several laboratory tests can help in diagnosing mitochondrial disease:
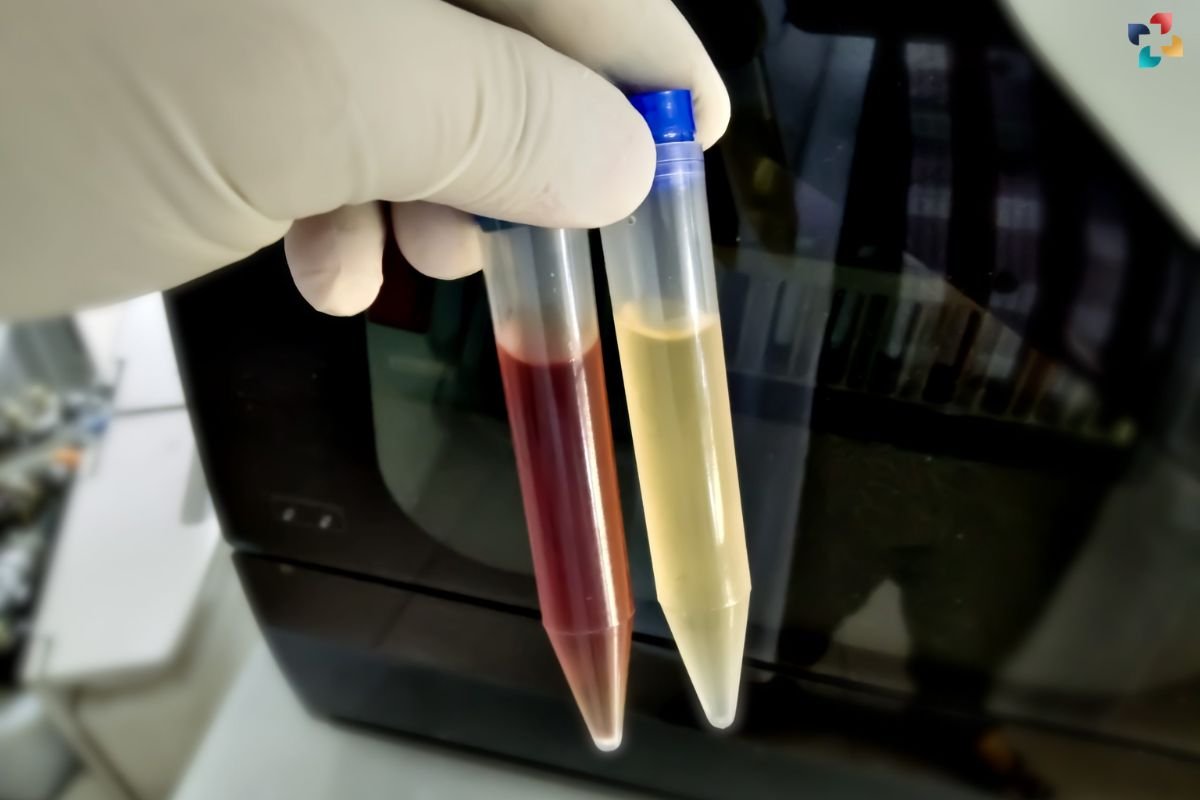
- Blood and Urine Tests: These tests can detect elevated levels of lactate, pyruvate, and other metabolites indicative of mitochondrial dysfunction.
- Muscle Biopsy: A sample of muscle tissue is examined for structural abnormalities in mitochondria and deficiencies in mitochondrial enzymes.
Genetic Testing
Genetic testing plays a crucial role in diagnosing mitochondrial disease:
- mtDNA Sequencing: Identifies mutations in the mitochondrial DNA.
- nDNA Sequencing: Identifies mutations in nuclear genes that affect mitochondrial function.
- Whole Exome or Genome Sequencing: Comprehensive genetic testing that can detect both mtDNA and nDNA mutations.
Imaging Studies
Imaging studies can help assess the extent of organ involvement:
- MRI and CT Scans: Used to evaluate brain and muscle abnormalities.
- Echocardiography: Assesses cardiac function and identifies cardiomyopathy.
Treatment of Mitochondrial Disease
There is currently no cure for mitochondrial disease, but various treatments can help manage symptoms and improve quality of life. Treatment plans are often tailored to the individual based on their specific symptoms and needs.
Symptomatic Treatment
Symptomatic treatment focuses on managing specific symptoms and preventing complications:
- Medications: Anticonvulsants for seizures, cardiac medications for heart issues, and pain relievers for muscle pain.
- Physical Therapy: Helps maintain muscle strength and mobility.
- Occupational Therapy: Assists with daily activities and adaptive techniques.
- Speech Therapy: Addresses speech and swallowing difficulties.
Nutritional Support
Proper nutrition is essential for individuals with mitochondrial disease:
- High-Energy Diet: A diet rich in carbohydrates and fats can provide the necessary energy.
- Vitamin and Coenzyme Supplements: Supplements such as Coenzyme Q10, riboflavin, and L-carnitine can support mitochondrial function.
Exercise
Regular, moderate exercise can improve muscle strength and endurance. However, exercise plans should be personalized and supervised by healthcare professionals to avoid overexertion and worsening of symptoms.
Mitochondrial Targeted Therapies

Research is ongoing to develop therapies that directly target mitochondrial dysfunction:
- Gene Therapy: Aims to correct genetic mutations causing mitochondrial disease.
- Mitochondrial Replacement Therapy: Involves replacing defective mitochondria with healthy ones, currently an experimental approach.
Clinical Trials
Participation in clinical trials can provide access to cutting-edge treatments and contribute to advancing research in disease. Patients should consult with their healthcare providers to explore available clinical trials.
Living with Mitochondrial Disease
Living with mitochondrial disease presents various challenges, but with proper management and support, individuals can lead fulfilling lives.
Multidisciplinary Care
A multidisciplinary care team is essential for managing mitochondrial disease. This team typically includes neurologists, cardiologists, geneticists, physical therapists, and other specialists who collaborate to provide comprehensive care.
Support Networks
Connecting with support groups and organizations can provide emotional support and practical advice for individuals and families affected by this disease. These networks offer a sense of community and valuable resources.
Education and Advocacy
Raising awareness about mitochondrial disease is crucial for improving diagnosis, treatment, and research funding. Patients and families can advocate for better resources and support by educating others about the disease.
Conclusion
Mitochondrial disease is a complex group of genetic disorders that affect the energy production of cells, leading to a wide range of symptoms and challenges. Understanding the causes, symptoms, and diagnostic methods is essential for managing the disease effectively. While there is currently no cure, various treatments and supportive measures can significantly improve the quality of life for those affected. Ongoing research and clinical trials offer hope for future therapies that may directly address mitochondrial dysfunction. Through multidisciplinary care, support networks, and advocacy, individuals with this disease can navigate the challenges and lead fulfilling lives.







