[Source – news-medical.ne]
A recent study published in eBioMedicine has revealed significant findings regarding population-wide immunity against COVID-19. Conducted in the Dominican Republic, the research involved a sample of 1,045 participants from an initial pool of 6,683, drawn from the Northwest and Southeast regions. The study aimed to understand the dynamics of antibody response against SARS-CoV-2, the virus causing COVID-19, at a population level, rather than the more commonly studied individual responses.
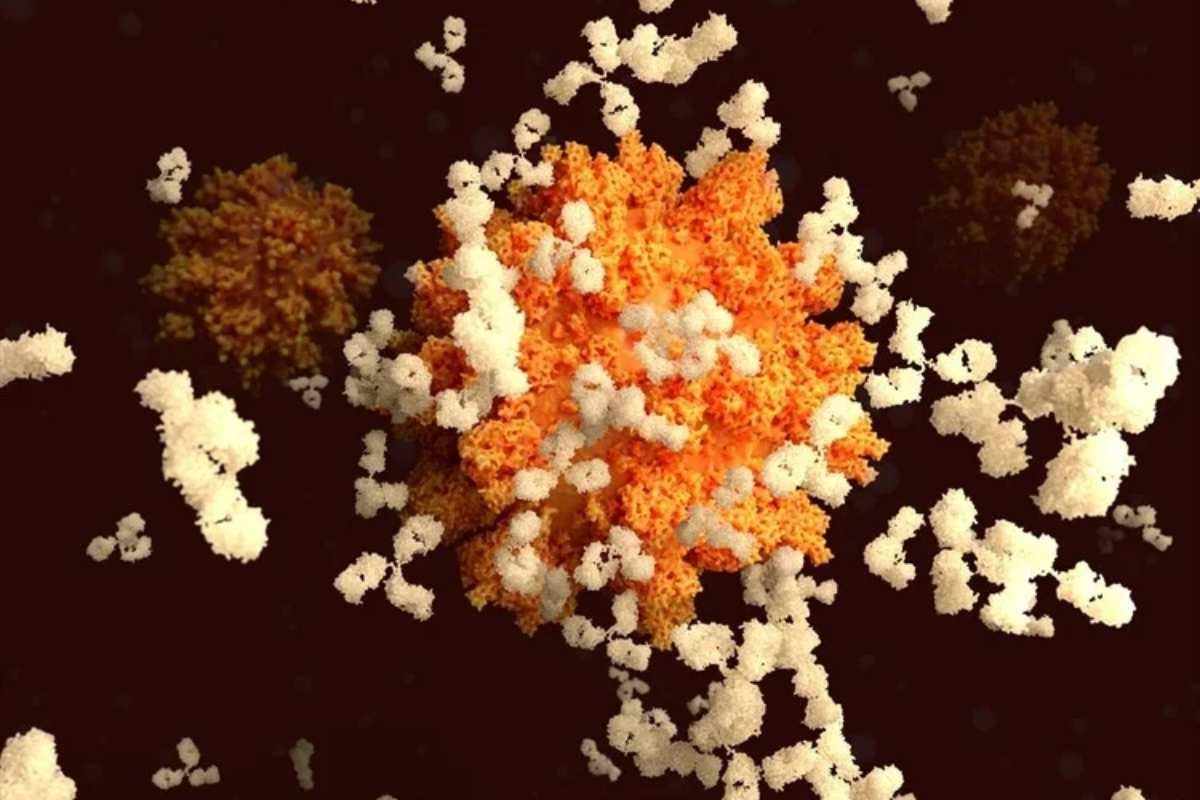
The researchers showed that despite variability in individual responses to infections and immunizations, population-wide antibody levels against the SARS-CoV-2 spike protein tended to converge toward a unique immune setpoint for COVID-19 antibodies. This convergence occurred regardless of the number of interim infections or vaccinations an individual experienced. The study found that individuals with antibody levels below this setpoint showed a gradual increase until they reached the threshold, while those with levels above it experienced a decline, eventually aligning with the population-wide average.
Methodology and Findings of the Study
The study was conducted in two phases, mid-pandemic in August 2021 and late-pandemic in November 2022, offering a comprehensive temporal view of the evolution of immunity across the population. The researchers used serological data to simulate changes in immune setpoint for COVID-19 indicators, specifically antibody titers against SARS-CoV-2 spike proteins. The data collection involved home visits where venous blood samples were taken, and electronic questionnaires were completed to gather information on demographics, medical history, vaccination status, and other relevant factors.
To analyze the data, the researchers employed a range of statistical methods, including Generalized Additive Models (GAMs) and machine learning classifiers, to compute changes in antibody titers over time. The study revealed a single-peak distribution of antibody levels, indicating that initially high antibody levels declined while initially low levels rose to meet the population-wide setpoint. The findings were consistent across various demographics, such as age, sex, geographic region, vaccination doses, and the number of infections, highlighting the robustness and generalizability of the results.
Implications for Future Pandemic Preparedness
The findings of this study have important implications for understanding and managing future pandemics. The concept of a population-wide “immune setpoint” challenges previous assumptions that population-level immune responses are random. Instead, it suggests that these responses follow predictable patterns, driven by underlying immuno-ecological pressures.
The study emphasizes the importance of “immunoepidemiology” in predicting disease spread and highlights the need for further research to refine these findings. Understanding the immune setpoint for COVID-19 antibodies could assist epidemiologists and policymakers in identifying possible pandemic-triggering diseases early on, allowing for the best deployment of resources and vaccinations to effectively combat disease spread.
While more research is needed to explore the theoretical underpinnings of these findings, this study represents a critical step in designing strategic public health responses and vaccination plans to better prepare for future COVID-19-like pandemics.