Craniocervical instability (CCI) is a serious and often debilitating condition that affects the structural integrity of the connection between the skull and the cervical spine. This instability can lead to a variety of symptoms, ranging from mild discomfort to severe neurological deficits. Understanding craniocervical instability, its causes, symptoms, diagnosis, and treatment options is crucial for those affected and the medical professionals who care for them. This article delves into the intricacies of craniocervical instability, providing a comprehensive overview of this condition.
What is Craniocervical Instability?
This refers to the abnormal mobility of the craniocervical junction (CCJ), which includes the base of the skull (occiput) and the first two cervical vertebrae (atlas and axis). This instability can result from various conditions or injuries that weaken the ligaments and structures responsible for maintaining the stability of this critical junction. When the CCJ is unstable, it can lead to compression of the brainstem, spinal cord, and nerves, causing a wide range of symptoms.
Causes of Craniocervical Instability

Several factors can contribute to this, including:
1. Traumatic Injuries
Trauma to the head or neck, such as whiplash injuries from car accidents or falls, can damage the ligaments and bones of the craniocervical junction, leading to instability.
2. Connective Tissue Disorders
Conditions like Ehlers-Danlos Syndrome (EDS), which affect the body’s connective tissues, can weaken the ligaments and lead to this. Individuals with EDS are at higher risk due to their inherently fragile connective tissues.
3. Degenerative Conditions
Degenerative diseases like rheumatoid arthritis and osteoarthritis can erode the joints and ligaments in the craniocervical junction, resulting in instability over time.
4. Congenital Abnormalities
Some people are born with congenital abnormalities that predispose them to craniocervical instability. For example, conditions like Chiari malformation can alter the normal anatomy of the craniocervical junction.
5. Infections and Inflammatory Conditions
Infections that affect the bones and ligaments of the craniocervical junction, such as osteomyelitis, can lead to instability. Similarly, inflammatory conditions like ankylosing spondylitis can contribute to this issue.
Symptoms of Craniocervical Instability
The symptoms of related to this can vary widely depending on the severity of the instability and the extent of neurological involvement. Common symptoms include:
1. Neck Pain
Persistent and often severe neck pain is a hallmark symptom of craniocervical instability. This pain may radiate to the shoulders and upper back.
2. Headaches
Chronic headaches, particularly at the base of the skull, are common. These headaches can be severe and debilitating, often referred to as cervicogenic headaches.
3. Neurological Symptoms
Neurological symptoms can include dizziness, vertigo, visual disturbances, tinnitus (ringing in the ears), and difficulty swallowing (dysphagia). Some patients may also experience cognitive difficulties and memory problems.
4. Weakness and Numbness
Instability at the craniocervical junction can compress the spinal cord and nerves, leading to weakness, numbness, and tingling in the arms and legs.
5. Autonomic Dysfunction
Autonomic dysfunction symptoms, such as irregular heart rate, blood pressure fluctuations, and digestive issues, may occur due to brainstem compression.
Diagnosis of Craniocervical Instability

Diagnosing this instability requires a thorough medical history, physical examination, and imaging studies. The following diagnostic tools are commonly used:
1. MRI and CT Scans
Magnetic resonance imaging (MRI) and computed tomography (CT) scans provide detailed images of the craniocervical junction, allowing doctors to assess the degree of instability and identify any structural abnormalities.
2. Flexion-Extension X-rays
Flexion-extension X-rays involve taking images of the neck in different positions to assess the range of motion and detect abnormal movement at the craniocervical junction.
3. Upright MRI
Upright MRI, also known as positional MRI, can be particularly useful in diagnosing craniocervical instability as it captures images while the patient is in an upright position, potentially revealing instability that may not be evident in traditional supine imaging.
4. Neurological Evaluation
A comprehensive neurological evaluation helps identify any deficits or symptoms related to this, aiding in the overall diagnosis and treatment planning.
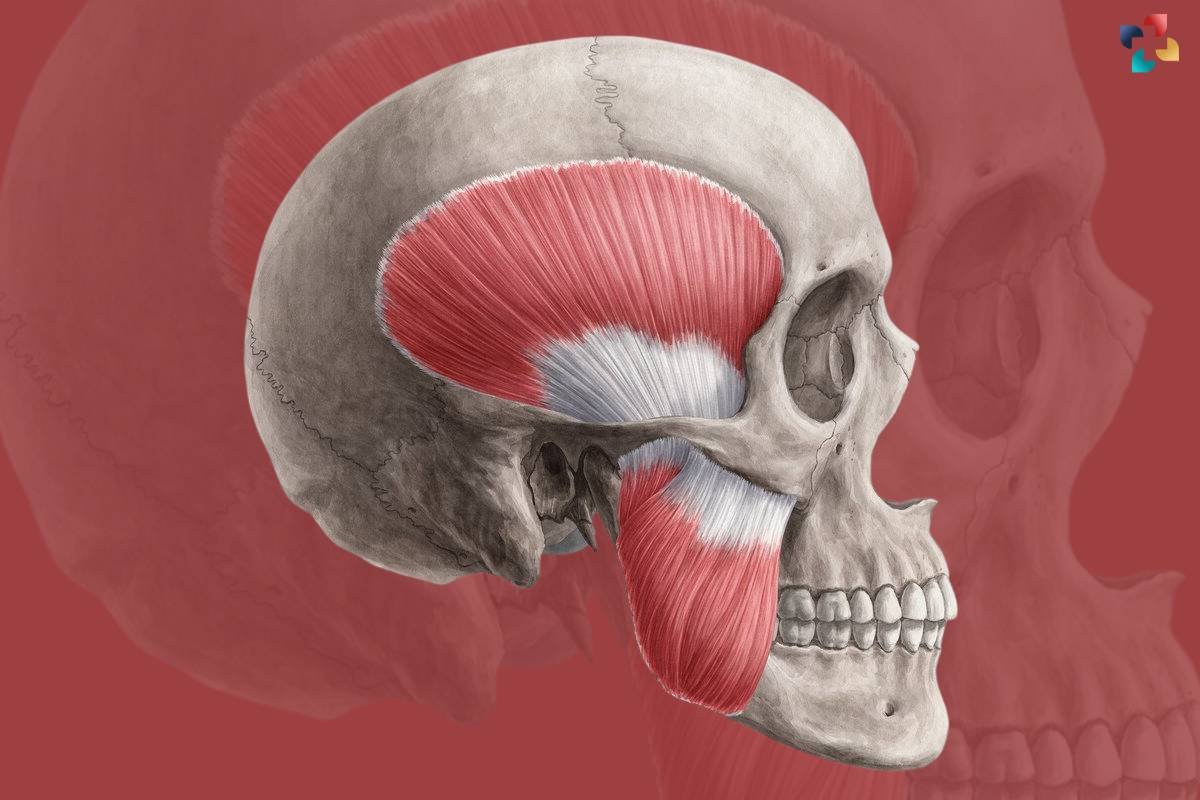
Understanding the Muscles of Mastication: Anatomy, Function, and Common Disorders
The muscles of mastication are primarily located in the head and neck region, centered around the temporomandibular joint (TMJ). In this comprehensive guide, we will delve into the anatomy, function, and common disorders associated with the muscles of mastication.
Treatment Options
The treatment of this aims to stabilize the craniocervical junction, alleviate symptoms, and improve the patient’s quality of life. Treatment options vary depending on the severity of the condition and the underlying cause. Common treatment approaches include:
1. Conservative Management
Conservative management may be suitable for mild cases of craniocervical instability. This approach includes physical therapy, pain management, and lifestyle modifications. Patients are often advised to avoid activities that exacerbate their symptoms.
2. Cervical Collar
A cervical collar can provide temporary stability and relief for patients with craniocervical instability. However, long-term use is not recommended as it can lead to muscle weakness and dependence.
3. Physical Therapy
Physical therapy focuses on strengthening the neck muscles and improving posture to support the craniocervical junction. Specific exercises and techniques can help stabilize the area and reduce symptoms.
4. Medications
Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and pain relievers can help manage pain and inflammation associated with craniocervical instability.
5. Prolotherapy
Prolotherapy involves injecting a solution into the ligaments of the craniocervical junction to promote healing and strengthen the ligaments. This treatment aims to improve stability and reduce pain.
6. Surgical Intervention
In severe cases, surgical intervention may be necessary. Surgical options include:
a. Fusion Surgery
Fusion surgery involves fusing the bones of the craniocervical junction to stabilize the area. This procedure is often performed using metal rods, screws, and bone grafts.
b. Decompression Surgery
Decompression surgery aims to relieve pressure on the brainstem and spinal cord by removing or reshaping bone or tissue. This procedure can help alleviate neurological symptoms caused by craniocervical instability.
c. Ligament Reconstruction
Ligament reconstruction surgery involves repairing or replacing damaged ligaments in the craniocervical junction to restore stability. This procedure is often used in conjunction with fusion surgery.
Living with Craniocervical Instability

Living with it can be challenging, but with appropriate management and support, patients can improve their quality of life. Here are some tips for living with this condition:
1. Follow Your Treatment Plan
Adhering to your treatment plan, including physical therapy exercises, medications, and any recommended lifestyle changes, is crucial for managing symptoms and improving stability.
2. Stay Informed
Educate yourself about craniocervical instability and stay informed about the latest treatment options and research. Knowledge empowers you to make informed decisions about your care.
3. Seek Support
Joining support groups or connecting with others who have craniocervical instability can provide emotional support and valuable insights into managing the condition.
4. Communicate with Your Healthcare Team
Open and honest communication with your healthcare team is essential. Keep them informed about your symptoms, progress, and any concerns you may have.
5. Prioritize Self-Care
Engage in self-care practices such as regular exercise, proper nutrition, and stress management techniques. Taking care of your overall health can positively impact your condition.
Conclusion
Craniocervical instability is a complex and often debilitating condition that requires careful diagnosis and management. Understanding the causes, symptoms, and treatment options for craniocervical instability is essential for patients and healthcare providers alike. With the right approach, individuals with craniocervical instability can find relief from their symptoms and improve their quality of life. If you suspect you have craniocervical instability or are experiencing related symptoms, consult with a medical professional to explore your options and develop a personalized treatment plan.







