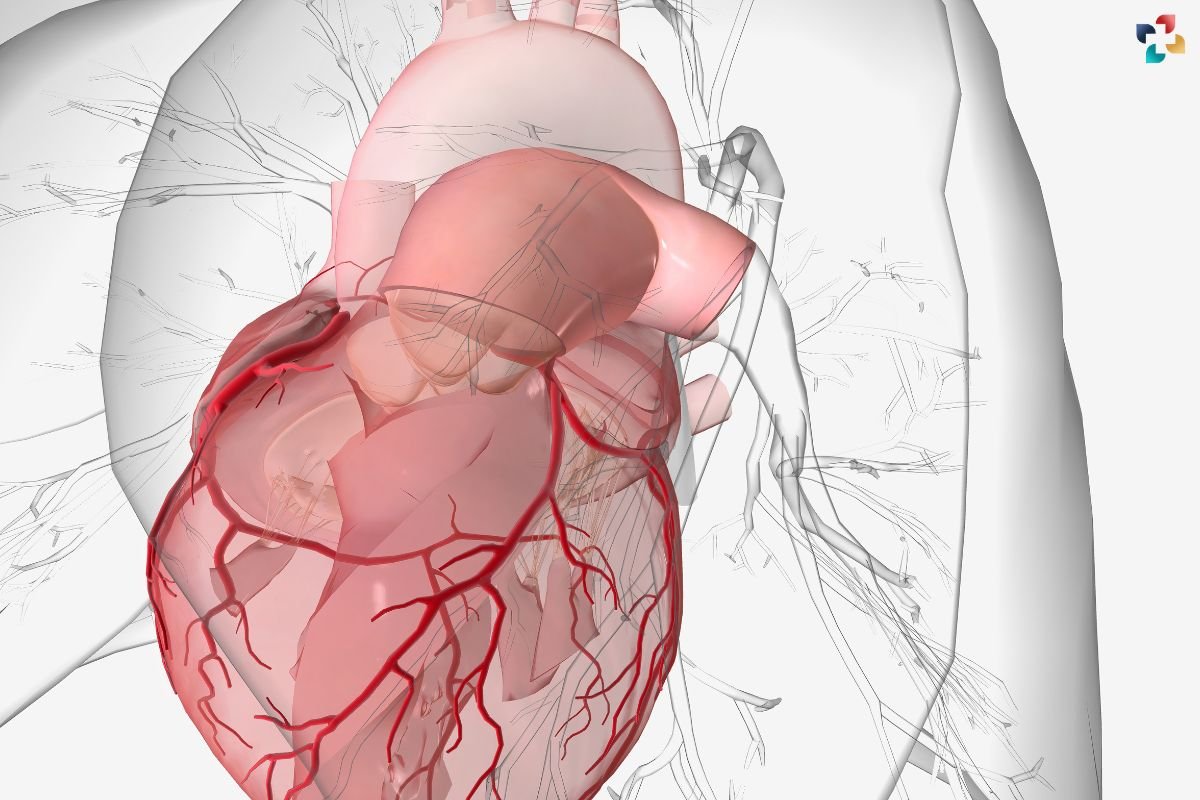
Ischemic cardiomyopathy is a critical cardiovascular condition that arises from compromised blood flow to the heart muscle, leading to impaired heart function. This comprehensive guide explores the definition, causes, symptoms, diagnosis, treatment options, and future directions in managing this condition.
Understanding Cardiomyopathy
What is Cardiomyopathy?
Cardiomyopathy refers to diseases of the heart muscle where the heart becomes enlarged, thickened, or stiffened, affecting its ability to pump blood effectively.
Types of Cardiomyopathy (Ischemic vs. Non-ischemic)
Cardiomyopathy can be categorized into various types based on causes and characteristics. It specifically results from coronary artery disease (CAD), which reduces blood supply to the heart muscle, whereas non-ischemic cardiomyopathy stems from other factors such as genetic mutations, infections, toxins, or autoimmune diseases.
Ischemic Cardiomyopathy Explained
1. Definition and Causes
It occurs when the heart muscle weakens due to reduced blood flow and oxygen delivery caused by narrowed or blocked coronary arteries. This condition typically follows from atherosclerosis, the buildup of plaque in the arteries supplying the heart.
2. Relationship with Coronary Artery Disease (CAD)
CAD, characterized by the narrowing of coronary arteries due to plaque buildup, is the primary cause of ischemic cardiomyopathy. As arteries become progressively blocked, the heart muscle experiences chronic ischemia, leading to damage and impaired function over time.
3. Impact of Ischemia on Heart Muscle Function
Ischemia deprives the heart muscle of oxygen and nutrients, resulting in myocardial damage and dysfunction. Over time, this can lead to weakened cardiac output and heart failure.
Causes of Ischemic Cardiomyopathy

1. Atherosclerosis and Coronary Artery Disease (CAD)
Atherosclerosis, a condition where fatty deposits accumulate in artery walls, narrows coronary arteries, and restricts blood flow to the heart muscle. This chronic deprivation of oxygen-rich blood contributes significantly to the development of this.
2. Myocardial Infarction (Heart Attack) and its Consequences
A heart attack occurs when a coronary artery becomes completely blocked, cutting off blood supply to a portion of the heart muscle. The resulting tissue damage and scar formation can weaken the heart’s pumping ability, leading to ischemic cardiomyopathy in the long term.
3. Chronic Ischemic Heart Disease
Chronic ischemic heart disease refers to ongoing reduced blood flow to the heart muscle due to persistent coronary artery disease. This chronic condition contributes to the progressive deterioration of heart function and the development of this illness.
Symptoms of Ischemic Cardiomyopathy
Common Signs and Symptoms
- Shortness of breath, especially during exertion or when lying flat (orthopnea)
- Fatigue and weakness
- Swelling in the legs, ankles, or abdomen (edema)
- Irregular heartbeats (arrhythmias)
- Chest pain or discomfort (angina)
Differences from Non-ischemic Cardiomyopathy
It presents with symptoms specific to reduced blood flow to the heart muscle, whereas non-ischemic cardiomyopathy symptoms can vary widely depending on the underlying cause, such as viral infections, genetic factors, or autoimmune disorders.
Diagnosis of Ischemic Cardiomyopathy
1. Medical History and Physical Examination
A detailed medical history and physical examination help identify risk factors and symptoms suggestive of ischemic cardiomyopathy. Family history, lifestyle factors, and previous cardiac events are crucial in assessing the patient’s cardiovascular health.
2. Diagnostic Tests (Echocardiogram, Cardiac MRI, Coronary Angiography)
Diagnostic imaging techniques like echocardiography and cardiac MRI provide detailed images of the heart’s structure and function, revealing abnormalities in heart muscle thickness, size, and pumping capacity. Coronary angiography is used to visualize blockages or narrowing in coronary arteries.
3. Biomarkers and Electrophysiological Studies
Blood tests measure biomarkers such as troponin levels, indicating myocardial damage. Electrophysiological studies assess the heart’s electrical activity, detecting arrhythmias and evaluating the heart’s conduction system
Treatment Options

1. Lifestyle Modifications (Diet, Exercise, Smoking Cessation)
Healthy lifestyle changes play a pivotal role in managing ischemic cardiomyopathy. A heart-healthy diet low in saturated fats and sodium, regular exercise tailored to individual capabilities, and smoking cessation reduce cardiovascular risk factors and improve heart function.
2. Medications (ACE Inhibitors, Beta-Blockers, Antiplatelet Therapy)
Medications such as ACE inhibitors, beta-blockers, and antiplatelet therapy help manage blood pressure, reduce heart workload, and prevent clot formation in narrowed arteries, respectively. These medications alleviate symptoms and slow disease progression.
3. Revascularization Procedures (Coronary Artery Bypass Grafting, Percutaneous Coronary Intervention)
Surgical interventions like coronary artery bypass grafting (CABG) or percutaneous coronary intervention (PCI) restore blood flow to the heart muscle by bypassing blocked arteries or opening them with stents, improving cardiac function and symptoms.
4. Implantable Devices (Implantable Cardioverter-Defibrillator, Cardiac Resynchronization Therapy)
Implantable cardioverter-defibrillators (ICDs) monitor heart rhythm and deliver shocks to correct life-threatening arrhythmias. Cardiac resynchronization therapy (CRT) devices synchronize heart contractions in patients with heart failure, enhancing pumping efficiency.
5. Advanced Therapies (Cardiac Rehabilitation, Heart Transplantation)
Cardiac rehabilitation programs provide supervised exercise, education, and support to improve cardiovascular health and quality of life. In severe cases of ischemic cardiomyopathy, heart transplantation may be considered for patients with end-stage heart failure.
Current Research and Future Directions

1. Emerging Treatments and Therapies
Ongoing research explores novel therapies such as stem cell therapy, gene therapy, and therapeutic angiogenesis to regenerate heart muscle, improve blood flow, and enhance cardiac function in patients.
2. Innovations in Ischemic Cardiomyopathy Management
Advancements in imaging technology, precision medicine, and personalized treatment approaches aim to optimize diagnosis, treatment outcomes, and long-term management strategies for ischemic cardiomyopathy.
Summary of Key Points
- It results from reduced blood flow to the heart muscle due to coronary artery disease.
- Symptoms include shortness of breath, fatigue, swelling, and irregular heartbeats.
- Diagnosis involves medical history, physical examination, imaging tests, biomarkers, and electrophysiological studies.
- Treatment includes lifestyle modifications, medications, revascularization procedures, implantable devices, and advanced therapies.
- Current research focuses on emerging therapies and innovations to improve ischemic cardiomyopathy management and patient outcomes.
Importance of Early Diagnosis and Treatment
Early intervention is critical in slowing disease progression, managing symptoms, and preventing complications associated with this, emphasizing the importance of regular cardiac assessments and timely medical care.
Hope for Patients with Ischemic Cardiomyopathy
Advancements in medical science and ongoing research offer promising avenues for enhancing treatment efficacy, quality of life, and long-term survival rates for individuals living with ischemic cardiomyopathy.
Conclusion
Ischemic cardiomyopathy poses significant challenges to cardiovascular health, but early diagnosis, comprehensive treatment strategies, and ongoing research offer hope for improving patient outcomes. Understanding the causes, symptoms, diagnosis, and treatment options is crucial in managing this complex condition effectively, enhancing quality of life, and promoting cardiac health.