In the ever-evolving landscape of interventional cardiology and vascular procedures, the development and adoption of innovative technologies play a pivotal role in improving patient outcomes and enhancing procedural efficiency. Among the array of advancements, vascular closure devices stand out as essential tools for achieving hemostasis and ensuring patient safety post-procedure. In this comprehensive guide, we delve into the significance, functionality, and benefits of vascular closure devices in modern healthcare settings.
Understanding Vascular Closure Devices
Vascular closure devices (VCDs) are specialized medical devices designed to achieve hemostasis and facilitate the closure of arterial access sites following diagnostic and interventional vascular procedures. These devices offer a minimally invasive alternative to traditional manual compression, reducing the time to achieve hemostasis, minimizing patient discomfort, and expediting ambulation post-procedure.

Vascular Closure Devices have revolutionized the management of arterial access sites, particularly in the context of percutaneous coronary interventions (PCIs), peripheral vascular interventions (PVIs), and diagnostic angiography procedures. By providing reliable and effective closure of puncture sites in arteries, Vascular Closure Devices have contributed to improved patient outcomes, reduced complications, and enhanced procedural efficiency.
In addition to their clinical benefits, Vascular Closure Devices offer economic advantages by reducing procedural time, length of hospital stay, and healthcare resource utilization. Moreover, they enhance patient satisfaction by minimizing post-procedural discomfort, facilitating early ambulation, and promoting faster recovery.
Applications and Indications
Vascular closure devices find widespread application in various vascular procedures, including percutaneous coronary interventions (PCIs), peripheral vascular interventions (PVIs), diagnostic cardiac catheterizations, and electrophysiological studies. They are particularly beneficial in cases where achieving rapid hemostasis is critical, such as in patients with coagulopathy, elderly individuals, or those at increased risk of bleeding complications.
Types of Vascular Closure Devices

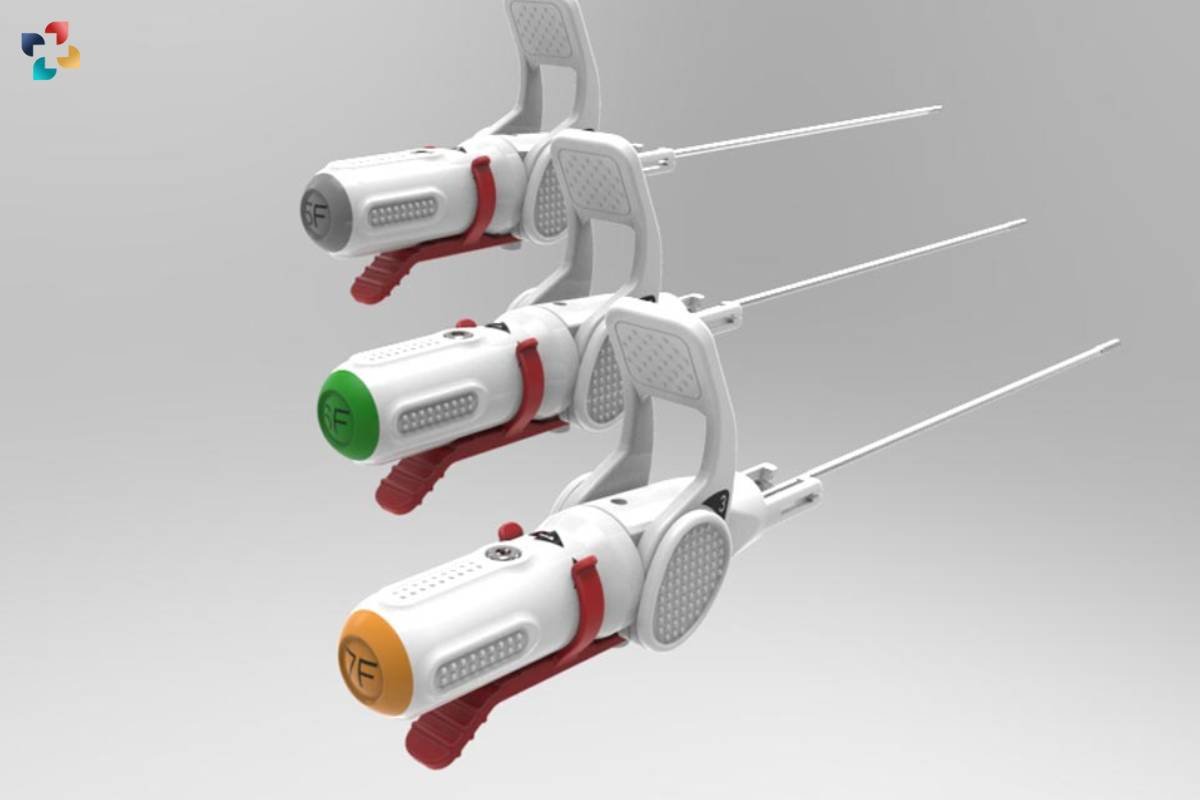
There are several types of vascular closure devices available, each offering unique mechanisms of action and advantages in terms of efficacy, safety, and ease of use. Common types of VCDs include collagen plugs, suture-based devices, sealant-based devices, and mechanical compression devices. These devices may be deployed through a variety of access site locations, including the femoral artery, radial artery, brachial artery, and dorsalis pedis artery, depending on the procedural requirements and anatomical considerations.
Benefits and Advantages
The adoption of vascular closure devices offers numerous benefits for both patients and healthcare providers. By facilitating rapid hemostasis and minimizing the need for prolonged manual compression, VCDs reduce the risk of access site-related complications such as bleeding, hematoma formation, pseudoaneurysm formation, and vascular injury. Additionally, they enable earlier ambulation and discharge, leading to enhanced patient satisfaction and reduced healthcare resource utilization.
Safety and Efficacy
The safety and efficacy of vascular closure devices have been extensively studied and validated through clinical trials and real-world experience. Overall, these devices have demonstrated comparable or superior outcomes compared to manual compression in terms of procedural success, time to hemostasis, rates of vascular complications, and patient comfort. However, appropriate patient selection, operator training, and adherence to device-specific instructions are essential to optimizing outcomes and minimizing complications.
Challenges and Considerations
Despite their advantages, vascular closure devices are not without limitations and considerations. Device-specific factors such as size compatibility, access site anatomy, and closure technique may influence procedural success and complication rates. Additionally, the cost-effectiveness of VCDs compared to manual compression remains a subject of debate, particularly in healthcare systems with budget constraints or reimbursement considerations.
Future Directions and Innovations
As technology continues to advance, the landscape of vascular closure devices is evolving to address unmet needs and improve patient care. Ongoing research and development efforts focus on enhancing device design, incorporating novel materials, and refining closure techniques to further optimize outcomes and expand the indications for VCD use. Additionally, the integration of adjunctive imaging modalities and hemostatic agents may offer additional benefits in achieving rapid and reliable hemostasis.
Conclusion
In conclusion, vascular closure devices play a critical role in achieving hemostasis and ensuring patient safety following vascular procedures. By offering a minimally invasive alternative to manual compression, these devices enhance procedural efficiency, reduce access site-related complications, and improve patient comfort and satisfaction. As healthcare providers continue to strive for excellence in patient care, the adoption and utilization of advanced vascular closure devices will remain integral to optimizing outcomes and advancing the field of interventional cardiology and vascular medicine.

Understanding Electrophysiology: Exploring the Intricacies of Cellular Activity
Essentially, the goal of electrophysiology is to clarify the intricate interactions among ion channels, membrane potentials, and neural signaling pathways in order to provide insight into the basic processes involved in cellular communication and function.
FAQs
1. What are Vascular Closure Devices (VCDs), and how do they work?
Vascular Closure Devices are specialized medical devices designed to achieve hemostasis and facilitate the closure of arterial access sites following diagnostic and interventional vascular procedures. They work by deploying closure mechanisms such as collagen plugs, suture-based systems, or mechanical clips to seal the puncture site in the artery, thereby preventing bleeding.
2. What types of procedures are Vascular Closure Devices used for?
Vascular Closure Devices are commonly used for percutaneous coronary interventions (PCIs), peripheral vascular interventions (PVIs), diagnostic angiography procedures, and other minimally invasive vascular procedures that require arterial access.
3. What are the advantages of using Vascular Closure Devices over manual compression?
Vascular Closure Devices offer several advantages over manual compression, including faster time to achieve hemostasis, reduced patient discomfort, enhanced procedural efficiency, and earlier ambulation post-procedure. They also minimize the risk of complications associated with prolonged manual compression, such as hematoma formation and vascular injury.
4. Are there any contraindications or potential risks associated with Vascular Closure Devices?
While Vascular Closure Devices are generally safe and effective, they may not be suitable for all patients or clinical scenarios. Contraindications and potential risks include arterial access site complications (such as pseudoaneurysm, arteriovenous fistula, or infection), allergic reactions to device components, and device-related malfunctions (such as failure to achieve hemostasis or device dislodgement).
5. How should healthcare providers select the appropriate Vascular Closure Device for a specific procedure?
Healthcare providers should consider various factors when selecting the appropriate Vascular Closure Device, including the type of vascular procedure, the size and location of the arterial access site, the patient’s clinical characteristics (such as vascular anatomy, coagulation status, and comorbidities), and the availability of specific device options (such as closure mechanism, device size, and compatibility with imaging modalities). Collaboration with interventional cardiologists, vascular surgeons, and other members of the multidisciplinary team is essential to ensure optimal device selection and procedural outcomes.







